CHAPTER THREE: DIAGNOSING DISC DISEASE
DAMAGE/PAIN SCENARIO
At the time, that fall on your buttocks when you were roller skating as a teenager, the football injury where the guy landed on you while you were falling backwards into a sitting position, or the time your back snapped forward in an auto accident, all seemed to be relatively insignificant injuries. However, they were importantly detrimental physiological and anatomical events. Some may have hurt for so little time that you hardly remember them, yet they were nevertheless capable of setting you up for a “Coup-de-Gras” later in life which (sounding familiar to many) goes something like this:
As an ageing human [your nucleus pulposus has solidified into a discus-shaped lump of cartilage], you wake up from a sound sleep in a soft bed [your Lumbar disc has been in flexion for nearly the last 8 hours] to recall that you forgot to take out the trash, and today is pick-up day. Unbeknownst to you, your desiccated nucleus pulposus has migrated to the end of the radial tear tunnel (fissure) that was created by past trauma to the spine and, as you raise your upper body off the bed to get up [you induce weight-bearing flexion that exerts nearly 500 lbs of force], you feel a slight twinge that you discount as insignificant [the disc material has just poised itself against the capsule]. You hurriedly trundle outside in your pajamas as fast as you can so as not to be seen by your neighbors. You are caused to lean slightly forward because its the most comfortable position [the disc material is exerting the fulcrum effect], and it is difficult to stand erect without slow adjustment which you don’t have time for just now. Still half asleep with the majority of your muscles remaining relaxed from your slumber and, therefore, providing no protection, you bend over, lifting the can that turns out to be a little heavier than you expected. So, you jerk it up–WHAM! [The last fibrous band of the annulus fibrosus ruptures, allowing the central disc material to be squeezed towards the edges of the vertebral bodies, pushing before it the thin ligamentous capsule with all its delicate nerve endings, herniating into and prolapsing the disc.] The pain takes your breath away, so you lean forward on the trash. The pain increases so rapidly that you can’t bear the weight of your own body; and you find that lying in trash isn’t so bad after all. You finally muster enough will power to try another attempt at erect posture. Now, the ground seems like the only site of solace. There, you can at least assume the fetal position and the grinding pain, like someone is using “the jaws of life” on the bones of your spine, is somewhat relieved just so long as you don’t move [any reduction in the load bearing on the disc reduces the hydraulic pressure on the peripheral ligamentous capsule]. You feebly call out for help but no one can do anything because the slightest movement results in agony. All that you can think to do is seek out medical care and prepare for the economic hemorrhage that is soon to come.
Your doctor can’t conceive of the possibility that you have herniated or prolapsed a disc because the lifting of a trash can in his mind isn’t sufficient force; so, in the absence of neurological findings you are diagnosed as having a “back strain,” given some pain pills, a few muscle relaxants, bed rest, some physical therapy, and told that it will get better. The only problem is that it doesn’t; and you are then faced with the task of figuring out what is wrong because you aren’t getting the answers you need and can’t see yourself living with this kind of pain for the rest of your life.
One needs to understand that a herniated disc is a mechanical problem; and mechanical problems have mechanical solutions. In order to solve a mechanical problem, you first have to determine physically where and what constitutes the mechanical lesion. When a disc goes “out,” it does so physically and, therefore, has a dimensional reality. It actually travels to another position that causes pain. In order to determine the best method or MANEUVER to put the displaced disc material back “in” to the center where it belongs, the location of the out-of-place disc material must be identified. The level of the vertebral column where the pain originates and the position of the fragment within the disc space must be fixed in the mind so that a mechanical strategy can be designed that will be both specific and effective. Before one can move a piece of matter, one must first know where the material exists in space.
There are expensive means of determining the location of a displaced piece of disc material; and there are self-administered, free, ways to accomplish the same task. The beginning of this section will briefly discuss the options available using standard, costly, diagnostic modalities ordered by licensed practitioners and the remainder will be dedicated to teaching the reader how to accomplish a “do-it-yourself” diagnosis. Taking the time to understand the options will assist the reader in making the best, most cost-effective decision. Without this understanding, the reader might end up spending thousands of dollars and getting nothing.
CONVENTIONAL DIAGNOSTIC METHODS
Understand at the outset, that medical science’s understanding of the causes of back pain is so limited that there, to this day, is no agreed-upon method of diagnosing a structural abnormality of the spine despite two extensive reviews in the medical literature.,
Nevertheless, when a patient presents with back pain to a chiropractor or physician, the most commonly ordered diagnostic imaging study is a spinal, plain film, X-Ray series. This usually amounts to long-axis side views, front to back views, and oblique views oftentimes focusing on the specific area of pain or the Lumbar region by virtue of its statistical probability of being the site of an abnormal finding. They cost Medicare $50; but, for everyone else, they can cost 2-3 times as much. Even more disconcerting is the amount of radiation to which the patient is exposed in light of how little they contribute to elaborating the cause of back pain.
People have a need to know how much radiation they will be exposed when “the routine X-Rays” are taken in an Emergency Room, the Chiropractor’s office, or when ordered by a physician. Undergoing a three view lumbosacral spine study is equivalent to having a Chest X-Ray study done every day for at least three years! This is one of the major reasons why a person should think twice before allowing themselves to be X-irradiated. A lot of people dispense with the risk by saying that we are always being exposed to radiation from natural sources. That is true, but there is a “natural” rate of cancer, too. Not only are you being forced to take your risks of getting cancer simply by choosing to live on this planet; but now when some other people on the planet want to make money off of you by increasing the amount of radiation you are exposed to by hundreds of times higher doses, I tend to get infuriated. Add to that, the doses calculated were probably measured with reasonably new equipment. Many facilities have purchased the old machines without image enhancing capability; and the doses are much higher. Evidently, the fact of radiation-induced genetic damage and its ability to cause cancer has escaped the educations of those people who down-play the 400 mRads of radiation to the female gonads and bone marrow entailed in every medically unjustified study they accomplish.
True, the cells of the body have a capacity to repair the genetic damage induced by radiation, however, that capacity has been evolutionarily designed to deal with background levels of radiation, not the logarithmic excesses to which some would have them exposed. Justification for the use of X-Rays (including CAT scans) exists, but it is limited by a few considerations which are pertinent to a patients decision to consent to an X-Ray procedure. Swedish investigators concluded that one might expect to find X-Ray evidence of a diagnosis not indicated by the physical exam in only one of every 2,500 adults under age 50 with low back pain. Many X-Ray findings are unrelated to symptoms of back pain and are found just as often in asymptomatic individuals.
If the first back pain episode started when a patient is over 50 years old or as a teenage athlete with activities strenuous to the Lumbar spine (i.e. gymnastics, wrestling, etc.) the yield of a plain film X-Ray study may justify the expense and radiation risk, especially if there has been a history of steroid use, a reasonable suspicion of ankylosing spondylosis, prior history of cancer, weight loss, bowel or bladder incontinence, a history of substance (drug or alcohol) abuse, significant trauma, failure to improve with conservative therapy within 4-5 weeks (The O’Connor Technique™ constitutes conservative therapy), or motor neuron deficits.
A condition that usually first affects athletic young people causing them to seek medical attention is called spondylolisthesis, which is often a congenital (present since birth) defect or traumatic fracture of vertebral pedicles (the pars interarticularis–the bridge-like bones that join the front portion of the vertebral bones with the back portion). When the segments are separated, it is called spondylolysis. Either can be painful or simply found incidentally during an X-Ray done for other reasons. That reality makes it a confusing problem to indict as the source of pain and also difficult to manage. This condition, however, is decidedly a statistical minority.
I mention this specific condition here because if you are one of the few people who have this condition I cannot be sure The O’Connor Technique ™ will be helpful. I doubt that it would be harmful because, in that event, the pain would not be helped by the technique and those patients would reasonably stop practicing it. In the worst case scenario, it might increase the pain, and logic would dictate that you would stop doing what hurts before any serious damage could be done. For more information on this condition especially as it relates to sports, go to the SPORTS Section of this book.
Another situation in which an X-Ray examination may reveal the source of pain is in the presence of pain that is constant, not improved by lying down, or does not respond to bed rest. These findings suggest a systemic disease or cancer. By “constant” it is meant that the pain stays largely the same regardless of what one does to try to alleviate it. Discogenic pain usually is reduced by lying down and returns when a person tries to get back up. If the pain were caused by cancer, no matter what one does, the pain of the tumor encroaching upon a nerve will not reduce in severity.
The other two most common diagnostic modalities used in the evaluation of back pain are the CAT Scan (Computerized Axial Tomography a.k.a. CT Scan) and the NMRI (Nuclear Mass Resonance Imaging a.k.a. NMR).
The CAT Scan is basically an X-Ray machine hooked up to a computer that takes lots of X-Rays, pools the information into one picture and gives an X-Ray cross-sectional slice-through- the-body. Because different tissues of the body allow X-Rays to pass more freely, those tissues with major differences in density can be differentiated from each other and not just bones are outlined. Its two largest draw-backs are the amount of radiation to which the patient is exposed and the limited resolution–especially in the neck region. To get some idea of how old the technology is, it was developed by money from The Beatles rock group. Since there are a lot of the machines still around and they have been paid off already, they can sell the images cheaper. But not even The Beatles can solve the radiation problem–it is even worse than that of the standard spine series. The problems of both cost and radiation can be somewhat mitigated by asking the physician ordering the study to limit it to just the painful area. Unless there is a compelling reason to irradiate the entire Lumbar region, you may reasonably request that the study be limited to just the painful area (which you can demonstrate to the radiologist). This way, if the pain is localized to one or two disc units your probability of seeing what is wrong by just examining those discs stands to be much more productive with respect to cost and radiation exposure.
CAT scans were once the best means of seeing into the spinal anatomy; but the NMRI is its higher-resolution competitor. The most accurate picture of the spine, especially the intervertebral disc structures, and least dangerous, is the NMRI (Nuclear Mass Resonance Imaging). It is about twice as expensive as the CAT Scan, but the resolution is much better without exposure to radiation. It actually is an amazing device. Patients are placed in a large magnetic field, and the manner in which the atoms of the body vibrate in that magnetic field differs from tissue to tissue and the difference can be detected with sensors. So, one gets a picture of the internal muscles, bones, cartilage, and other soft tissues. Whereas the plain X-Ray only sees the bones, with an NMRI device, the displaced disc material can actually be seen; and the position of it relative to the vertebral bodies and, more important, the spinal nerves can be determined.
The draw back here is the cost. It is a relatively new technology and expensive. If you are paying for it, you are looking at upwards of a thousand dollar bill. That’s a pretty hefty sum, and it is very difficult to get a doctor to order one because they are hassled and intimidated by HMO’s, administrators, or third party payers’ refusal to pay. Or worse, the managed-care doctor himself (when your health care dollars are paid to him and capitated in advance) can have become reluctant to spend his “own” money on you. The conflict of interest inherent in capitation warrants an entire book; but, suffice it to say, that, if you are in a capitated care plan, this book is probably the only way in which your back will be made to get better. When anyone is getting paid more by delivering less care to your back, it will probably get better on its own before they do anything that can realistically be expected to alter the outcome.
The most common justification they give for not ordering any expensive modality is that at any given time, probably 20% of “normal” thirty-year-olds who undergo an imaging study (CT, myelogram or NMRI) can be shown to have asymptomatic evidence of herniated discs. This statistic is then often misused to justify a belief that the finding of an herniated disc on an imaging study is not equated with pain. I fervently disagree. The presence of a herniated disc on an imaging study constitutes irrefutable evidence that the patient has suffered an injury to the disc system; and the burden of proof, then, rests upon the physician to prove that the disc is not responsible for the pain’s origin. Until that is done, the disc should be considered the most likely source until it is proven that such is not the case. Admittedly, this advice deviates markedly from the current approach to back pain management; yet I am convinced that, as the reader completes their understanding of The O’Connor Technique™, they will logically conclude that it exposes a fundamental inadequacy in the current “academic” approach to this human problem.
The finding that a substantial percentage of asymptomatic people are usually found with evidence of a herniated disc simply establishes the reality that far greater numbers of people (than currently believed) could be suffering from disc disease. These people simply may not have had the diagnosis made previously. That doesn’t mean that they don’t have disc herniations, it just means that they don’t have symptoms at the time of the study. Any time a “scientific” study establishes the statistically significant presence of undiagnosed disease, it is equally probable that the explanation rests in a failure of the diagnosticians to have previously elaborated the disease through adequate histories and physical examinations.
Many patients may have unconsciously, unknowingly, or coincidentally accommodated to the problem by limiting their activity, become so accustomed to the pain and limitations of movement that they no longer accept or perceive it as abnormal, stopped complaining about it to themselves or their physician’s, or the area has become scarred down and physiologically, spontaneously, stabilized. Denying the significance of a disc herniation does not, however, make it go away or provide assurance that it will not again become symptomatic later.
The event that caused the herniation also could be so distant in time that a recollection of the event is difficult; but it is these very types of patients who probably constitute the population of persons who (seemingly inexplicably) are immobilized by pain when the already herniated disc only requires a relatively small amount of force to push it into a painful configuration. These are the type of patients who give a history to their doctor that they were simply taking out the trash or sneezing when suddenly they were immobilized by pain. The doctor feels the area, finds muscle spasm and assuming that the force described could not have been sufficient to cause a herniation, then erroneously concludes that the source of the pain is a pulled muscle–which is now in spasm. They then conclude that no imaging study is necessary with that diagnosis and elect the cheapest and easiest strategy: “conservative management” (which is no more than what we physicians call “benign neglect”) relying upon the assumption that within two months most of these patients will again be pain-free.
You may find it difficult to obtain an NMRI if your doctor’s compensation is capitated by your insurance or health care program because the doctor is now spending his money. This whole movement in medicine called “managed care” is the worst of all systems from a quality point of view because an inescapable conflict of interest is designed into it. If your doctor is paid up front to take care of you, when it comes to ordering an expensive study or sending you to a specialist–the money comes out of his pocket. As perverse as it may seem, human nature being what it is, don’t expect your doctor under that type of system to do anything but the cheapest management possible unless he is a Saint. The most important factor influencing his decision appears to be how much risk he is willing to take with your well-being yet still not get sued.
This book is not the ideal forum to expose the particulars about how bad the basic philosophy of these HMO’s, Kaiser-like plans, or capitated programs truly are because that’s another entire book that belongs more in the horror stories section of the book store. But it is appropriate to address the motivations of those persons charged with the responsibility of your health because, when it comes to the costs relegated to back pain, those paying for the care do not want to spend any more money than is absolutely necessary. It seems that everyone is jumping on the “get-it-done-cheaper-at-any-cost-band-wagon” and, those that don’t climb aboard of their own volition, are being economically drummed out of the practice of medicine by the administrators and business people who are reaping enormous profits from this scam (right now, their “take” averages 12% of the health care budget in any market they can capture). It is accurate to say here, that if the “bean-counters,” whether at a governmental or corporate level, can persuade a doctor not to order an expensive test, they can take that money and give it to themselves. So, more often than ever before, beneficial (and even essential) diagnostic information is not obtained because someone along the line is willing to play the odds such that, by withholding any particular procedure or diagnostic test, they can stumble along without it (regardless of the excess pain and prolongation of ignorance that such a strategy entails) so long as they are willing to sustain the reality of you not getting better, staying in pain longer than necessary, or suing them.
An excellent example of this mentality is represented by a recent case known to me. JM is a physical laborer who sustained a fall and has never been able to alleviate the back pain subsequent to that trauma. Two years after the injury, he presented with obvious clinical symptoms of disc prolapse with possible spinal nerve root involvement at the clinic where I practice. I attempted and then taught him some self-administered extension maneuvers to see if he would benefit, but he not only achieved no obvious relief, but he had to stop doing them because they hurt more.
The degree of pain involved and the potential presence of nerve root impingement indicated that the safest and most prudent course would be to acquire an NMRI to make certain that he could mobilize the spine by without risking additional nerve damage. When I ordered the NMRI, a nurse with absolutely no knowledge of the specific patient or back pain in general refused the imaging study and insisted that he go to an orthopedist specialist for consultation. Because the local Medicaid managed-care organization refused to pay local orthopedists a reasonable compensation for their work, he was sent to the University where he was seen by a student doctor. Without knowing whether the patient had a partial extrusion that could reasonably be expected to be made worse by extension exercises (a risk I was unwilling to take in light of the fact that extension was so painful), he ordered physical therapy with extension exercises before determining the extent of the protruded disc material with an NMRI. This was done in the presence of the fact that in my consultation request I informed the doctor that previous extension-type physical therapy attempts had met with a worsening of the condition.
It seems now-a-days, that economics are the most influential determinant with regard to whether an NMRI is “necessary.” An NMRI costs about $1,000.00. The physical therapy costs $60 a week. If he’s hurt by the exercises, it helps convince a physician that the fellow has a real problem–the pain and neurological function gets worse. Then, only after his condition gets worse or no better will some other strategy be tried. The problem with this scenario is that JM unnecessarily must be put through weeks of pain before being “allowed” the imaging modality and risk suffering a permanent neurological deficit when treated by an exercise instructor who has no true knowledge of the injury’s extent. In fact, even the doctor doesn’t know it because he failed to obtain the “road map” NMRI. So, I was forced to stand by and watch this man’s future ability to walk jeopardized because money wouldn’t be spent by a nurse (whose job is to refuse services) and the doctors within this system were willing to proceed with a demonstrably dangerous plan from a perspective of elective ignorance. The frequency with which this occurs is so great that it defies description; however, I present it so that the reader will at least be forewarned about the current state of affairs in medical management decisions and be better prepared to deal with it.
My solution was to send a letter to his lawyer, outlining the problem, and to the doctor reminding him that extension exercises were already unsuccessfully attempted and persisting with them presented the potential for further harm. In that way, the entity that chooses not to do the proper imaging study will have a legal “sword of Damocles” hanging over its head (rather than mine). You see, when capitated health plans deny services, the legal liability for that decision still remains with the physician unless he makes a good-faith effort to protect the interests of his patient. I protected my patient while at the same time transferring liability away from myself. If the other physician is so arrogant as to persist with his plan to proceed blindly, he would be the one to end up in court explaining his methods to a jury. My ethics won’t allow me to violate the trust engendered in the physician’s precept primum non noicere (first do no harm) nor ignore the published guidelines that justify an imaging study if the patient has gone greater than six weeks without alleviation of symptoms. However, health plans are not governed by that creed and can choose to ignore any given M.D.’s orders. Their interest is in acquiring wealth regardless of patient’s additional suffering or risk. The reality is that these machinations exist so far beyond the understanding of the patient that the administrators can get away with just about anything. They act upon the assumption that their decisions will not be legally questioned until it can be proven, afterwards, that they caused damage. Even in the presence of damage, it is very hard to prove that they actually caused the damage, so it behooves the patient to become sufficiently educated to manage their own back problem through the system, to prevent irrevocable damage. I designed this book for laypersons because they must be able to make their own diagnosis.
Don’t mistake my loyalties, most physicians I have met are hard-working, humanitarians with altruistic goals and genuine concern for the welfare of their patients. However, as hard as it may be to believe, (because doctors are sometimes seen as “all-powerful”) they are often victims of forces beyond their control. In that instance, few of them are martyrs enough to suffer in your stead. All too often, they, by their own experience with “the system” have become complacent and unwilling to stand up for their patients’ well-being let alone their own.
Here’s how it works. If a particular capitated program’s cost-control officer looks at the statistics and sees a particular physician is ordering too many NMRI’s, he will be either intimidated into ceasing this practice (by volumes of additional paperwork, “guideline” educational seminars, demands for specialty referrals, or “de-credentialed” if he persists. These capitated plans and HMO’s usually have clauses in their contracts that allow them to remove a doctor from their provider lists “without cause.” To even the best doctors, this can mean being put out of business. It is a modern form of corporate “Black-Listing;” and it especially happens to doctors who “cause trouble” when they protest decisions of the health care plan not to approve expensive procedures. If you suspect you are suffering this situation, don’t attack your doctor, write a certified letter to the healthcare plan demanding an alternative decision. By demanding that they put in writing the specific criteria they are using to deny you that service and indicating that any future pain, suffering, or disability resulting from a failure to adequately diagnose the problem, you intend to hold the persons making the decision liable for damages because, inherent in the act of refusing legitimate diagnostic or therapeutic modalities, they are practicing medicine without a license.
If your back pain is not getting better and, after practicing The O’Connor Technique™ enough to convince yourself that you have given it an adequate opportunity to work, you feel that having an anatomical image of the problem will make the definitive diagnosis, and you are paying for it yourself (or have a doctor that is paid up-front by your health care plan that refuses to order the study), there may be a compromise. You can reduce the cost by specifically asking your doctor to order just a limited study of the area in question. Usually, the painful area of the spine only involves a few segments and, after you have lived with the pain for a while, it is not too difficult to determine where the specific area of the spinal pain is located. It is unnecessary to image the entire spine when only a small area is actually affected by pain. So, if you want the best imaging study to determine if a disc is herniated, a limited NMRI may be the best option. By reading on, you will be given a means to localize the site of the problem if an NMRI or CAT scan becomes necessary.
However, the greater purpose of this book is to teach the reader how to make their
own back better. In large part, that must include figuring out, for yourself, without great expense, what is actually wrong. The following describes how you can do it yourself because, in fact, you are the best person to do it. No doctor known to me is aware of this method, nor is it, to my knowledge, described in the medical literature (and believe me, I am well-read in the field of back pain); so, up until now, patients have really been left to their own devices, anyway. So, at worst, the situation hasn’t changed with the advent of this book. At best, the reader has every reason to believe that they, themselves, can be made competent enough to figure out if they have a disc problem and remedy it by a few simple movements.
SELF-DIAGNOSING YOUR DISC
I am convinced, through experience teaching The O’Connor Technique™, that, for the average person with back pain, it is possible for a patient of normal intelligence with no medical training to identify, without expensive modalities, the exact origin and site of the pain and thereby learn to make their own diagnosis. This is done by performing specific movements of the spine and focusing on what happens to the pain. These movements can be categorized and technically defined as a Diagnostic Circumduction because the movements employed constitute what is known in anatomical or orthopedic parlance as “circumduction.” Based upon a knowledgeable and logical deductive reasoning process, anyone properly educated can arrive at their own diagnosis by engaging in Diagnostic Circumduction and, thereafter, identify the exact location of their displaced disc material so as to, later, be able to manipulate it back into the pain-free configuration.
This method of Diagnostic Circumduction to diagnose a disc condition is so successful for me in my practice that, many times, I get an NMRI (Nuclear Mass Resonance Image) or CT scan simply to confirm my clinical diagnosis. I seldom find a major discrepancy between the image study and my clinical exam, except in the presence of spondylolisthesis.
Now, the reader may scour the existing medical literature on back pain in search of the clinical term–Diagnostic Circumduction. To my knowledge, it does not exist outside of this book, and I have been specifically exploring back pain literature for well over 15 years. Moreover, no mention of Diagnostic Circumduction is made in the newly published government guide to back pain management which, by virtue of its “definitive” auspices, should contain it or a similar test if it exists. Therefore, when Diagnostic Circumduction is used by professional clinicians to diagnose a disc herniation, in the absence of alternative nomenclature, it can best be referred to as “The O’Connor Test“. If it can be shown that some other author described it prior to 1990, I would gladly re-title it; however, until such time, I will continue to represent it as my contribution to clinical medicine.
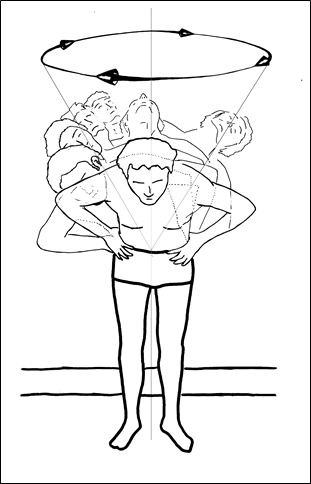
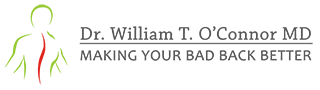
Figure 1; Circumduction at Lumbar spine.
In developing this technique, I discovered that, whenever a person with back pain attempts to circumductionally pivot (as in Figure 1) the spine at a particular vertebral level where disc material is herniated and significantly displaced, they almost invariably experience pain that has an arresting component to it. That is, their circumduction is physically stopped by the obstruction caused by the displaced disc material. As they circumduct through that particular arc where decentralized disc material is located (almost always in the extended configuration), they begin to trap, pinch or put pressure on the disc material that is off-center; and a very specific pain is produced that is easily distinguishable from other types of pain. This pain, as described in the previous chapter is due to the fulcrum effect. It is a pain that stops movement as though an actual object was physically obstructing the movement, not highly unlike a pencil had been put in a door hinge and the door attempted to be shut. One can’t continue to force the door shut without breaking something. Similarly, when one tries to gyrate through a point between two vertebrae where a piece of disc material is de-centralized, one cannot complete the circumductional movement while maintaining the same degree of lateral bending or extension. When this action is attempted, the person with a decentralized disc feels something like a wedge is stuck in the way. This is the sensation that frequently is described as a “catch,” as if something were “stuck” in the back or something in the back “went out.” The sufferers almost uniformly feel as though, if they could just move in the right way, the pain would resolve or the back “go back in.”
The pain more often than not feels like an object is stuck in the spine at a fixed point. Every time the person rotates the painful area of the spine through circumduction and reaches the same area where the wedge is stuck, they have to stop or the pain becomes too great. Either way they circumduct, (clockwise from left to right or counterclockwise from right to left) upon reaching approximately the same point where the disc material is herniated, they are arrested in their range of motion by pain. The person senses that if they persist in the circumduction without reducing the degree of lateral bending or extension, the pain will become unbearable. So, in order to continue circumducting, they have to relax the degree of extension (or leaning) over the site of the herniation by dropping the hip, bending the knee on the same side of the pain, or straightening up slightly to reduce the degree of lateral bending or extension. Once this is accomplished, the circumduction can usually be continued unimpeded because by so doing, they are shifting the center of gravity at the problem disc to a configuration wherein the vertebral bones are no longer putting fulcrum-like forces on the displaced disc material.
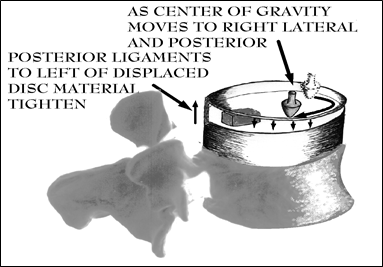
Figure 2; Fulcrum effect causing pain as circumduction proceeds clockwise until arrested by displaced disc material.
After they adjust their center of gravity so that the increased pain is no longer present, the usual background pain may still be present; and, no matter how many times they try, the range of motion through that same part of the arc at the particular spinal level is repeatedly and reproducibly impaired. What is happening has been anatomically described in Chapter 2 as the Fulcrum Effect.
Often, when a person is circumducting and they come to the point of restricted range of motion, they often will automatically bend the knee on the painful side so as to drop the hip and thereby reduce the degree of lateral bending. When I am examining a patient I sometimes move their upper body in such a way that maintains the degree of lateral bending and extension and doesn’t allow them to try to return to the neutral position. This forces them to bend their knee or drop their hip to avoid the pain, and it is a sure sign that I have identified the site of the disc displacement. The presence of an arrest in circumduction might properly be termed a “POSITIVE O’CONNOR TEST” in medical parlance since, to my knowledge, this distinction has never been made before in the medical literature.
The pain is generated by the same type of forces that strain the hinge when an object prevents a door from closing. A long moment arm is acting on a very small fulcrum-to-object lever arm length. In the disc’s case, the hard, displaced, disc material is acting as the fulcrum, the vertebral body and the adjacent disc component above and anterior to the displaced disc material is the long moment arm, and the ligaments that hold the vertebral bodies together are equivalent to the “objects” moved by a fulcrum when it operates. Just as a long pry-bar can lift a heavy stone, similar force applied to tighten such short ligaments results in pain. (See Figure 2)
In order to discover where the displaced disc material is actually located along your spine, you need to learn how to perform a Diagnostic Circumduction in which you attempt to circumduct in a leaning flexion that progresses clockwise or counterclockwise to an extension such that the body is pivoting at the disc unit level where the spine is most painful. This is done by first leaning forward slightly (flexing) such that the body is bending exactly at the site of spinal pain. Ideally, the area below the pain should stay immobilized as best as you can and only the vertebrae above it should be allowed to engage in circumductional motion.
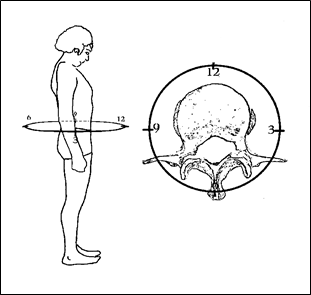
Figure 3; Clock face superimposed upon body and vertebral bone for orientation.
To understand how to perform a meaningful Diagnostic Circumduction on yourself as well as how the designation of clockwise and counterclockwise is used in this book, you need to view (in your mind’s eye) a clock face from a perspective such that you are looking down upon the clock as though it were superimposed upon the vertebral bodies in such a manner that the plane of the clock face is parallel to a cross-sectional view of the disc. The clock is superimposed upon the spine such that the vertical (up and down) axis of the spine transects the center of the clock. The plane of the clock face should be horizontal and perpendicular to the axis of the spine. For practical purposes 12:00 should be directly in front of you. The 6:00 position would, understandably, be directly behind you, and 9:00 would be on your left.
Depending upon what particular disc unit of the spine you are addressing, the plane of the clock can be elevated or lowered in your imagination; but it should always be kept perpendicular to the plane of the spine. The intricacy of this designation is not important. What is important is that you develop some way of orienting yourself to some conventional diagram for the purposes of this discussion and future reference because, if properly aligned, the horizontal plane of the clock face is superimposed upon and parallel to the horizontal plane of the discs (See Figure 3). It is as if the problem disc now has clock face numbering system superimposed upon it so its reference points can be discussed and the reader can be directed without confusion.
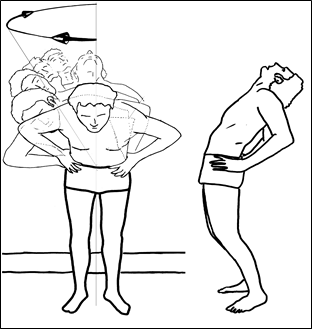
Figure 4; Circumduction to right (clockwise) ending in full extension.
Now, to perform a Diagnostic Circumduction, start by facing towards the 12:00 position on the clock, putting your hands on your hips for balance and support, and mildly lifting your upper body off of your lower body by pushing inferiorly with your arms (this takes some hydraulic pressure off of the disc and makes it easier to know which pain is acting); then flex anteriorly (flex approximately 15 to 20 degrees but no greater than 30 degrees forward off of an upright posture). If you flex forward too much, that will increase the prolapsing pressure and unnecessarily increase the pain. One way of knowing if you are flexing the right amount, flex forward (anteriorly) until a stretching pain comes to your back, then back off (reduce the amount of flexion) until that pain stops.
Leaving your feet firmly planted at about shoulder width, begin smoothly leaning/circumducting (not twisting which is technically termed axial rotation) only that portion of your body above the painful site in one direction or the other. If the pain seems to give you more symptoms to one side or the other then start circumducting towards that direction.
For this example, I choose to circumduct clockwise (to the right) first, pivoting at the level of a lower Lumbar disc. So, begin to tilt towards the 1:00 position (clockwise) while keeping the angle of the upper body at the same degree of flexion. The leaning is continued by a tilting of the body above the pivot site to this same side while eventually you will be moving from flexion to extension. You should be only allowing the spine superior to the site you are pivoting around to flex or extend, the segments below the site should be kept in neutral position. When you start circumducting to the right, you lean more and more to the right; and, in a smooth continuous motion, you progressively circumduct in an arc, a little more each time by leaning more to the right and posteriorly until at the end of the movement, it is as though you were leaning backwards in full extension (as in Figure 4).
Since this may be difficult to understand, I will elaborate in other words. At the level of the spine where the pain is located, try to make your spine bend or lean enough to reproduce the same-sided pain you are usually experiencing with movement. About 15 to 30 degrees off the axis of a normal erect posture should be sufficient. While keeping this same degree of tilt, slowly and carefully make a gyrating-like rotational movement (like a gyro-scope or a top when it begins to run out of energy and begins to carve out an inverted cone in space) so that, by the time you progressively circumduct to the 3:00 position, you are in effect leaning sideways to the right as much as you can without losing your balance. This Diagnostic Circumduction is not to be confused with twisting. You are not twisting the spine during this test. Continue this same movement towards the 4:00 position. You may at this point have to thrust your hips forward (like you were sticking out your belly-button) at this point to keep the center of gravity of the upper body over your legs. If your back pain usually gives you pain more on the right side of your body this means that the disc is herniated more to the right than directly in the posterior midline; so, somewhere between about 3:00 and 6:00 the pain should begin to increase so much as to prevent you from circumducting further without straightening up slightly or dropping the right hip or bending the knee to allow the movement to proceed. If your motion is arrested, what is arresting your motion is the off-center displaced disc material that has begun to act as a fulcrum; and, as the peripheral portion of the vertebral bodies progressively compress from the 3:00 to 6:00 positions on the periphery of the disc, they begin to compress and pinch the displaced disc material, forcing it to act on the intervertebral ligaments with a fulcrum effect (review Figure 2 here and Figure 32 in Chapter 2) and creating increased pain to the point where you have to stop. The obstruction caused by the displaced disc material makes continued circumduction in extension, in this manner, realistically impossible. If the disc is “out” (by that I mean that it is displaced enough to impede circumduction in extension, you should not be able to accomplish full extension over that point of herniation without experiencing pain. I have termed this phenomenon Arrested Circumduction in Extension, in this case, Arrested Circumduction in Extension to the right.
The pain that Arrests Circumduction in Extension should have a mechanically obstructive character that makes it feel as though something were physically blocking the ability to circumduct further. That is, you sense that if you continue the motion without decreasing the angle at which you are leaning or extending, the pain will be markedly increased, possibly even unbearable. When this happens, don’t force it further, you are just establishing the diagnosis of a de-centralized piece of disc material, herniation, prolapse, or protrusion and testing the right-sided margin of the disc bulge at this point.
As a side note, this is the type of sensation that patients routinely describe as a “catch,” or their back is “out” or “stuck.” They also agree that it feels like if they could just move the right way the pain would be relieved. If this is the sensation you feel, you are doing the test properly. When your clockwise circumduction is halted by this obstructing pain, you have just identified the position of the right margin of the displaced disc material.
In most cases, you will be stopped in your movement to the right (or clockwise) before reaching the region of the posterior midline. Then, you continue The O’Connor Test by repeating the movement to the left (or counterclockwise) by starting from the front again and, only this time, successively perform the flexion, abduction, extension, and adduction in sequence to the left which similarly brings you around leaning progressively more posteriorly until finally you are leaning backwards. To do this, go back to the 12:00 position and repeat a similar leaning/gyration-like movement in the opposite direction as before. This time, move to the left (counterclockwise) by continuously leaning/circumducting to the 11:00 position then on to 10:00 position, and so on. As you did before, continue to smoothly circumduct and thrust your hips gently forward when you get to the 9:00 position if necessary. As you go from 9:00 on towards 6:00 and the back begins to assume an extended posture, the pain should be elicited at some point in the circumduction before reaching the posterior midline if the disc material is herniated predominately to the left. Similarly when you moved in a clock-wise direction, your movement should be arrested by pain when you reach the point where the pressure created by the two vertebral body’s edges begin to apply force to the herniated disc material. The point that now stops you defines the left margin of the displaced disc material.
If your pain is predominately one sided, (and for the purpose of this example I will assume that it is more to the right) one should notice that the movement counterclockwise is not arrested until circumducting somewhere well beyond the 9:00 position. It will usually become arrested again at least when one approaches the 6:00 position (the posterior midline) from a counterclockwise direction because the vertebral body’s peripheral margins will be compressing the other side of the herniated material as the diagnostic circumduction proceeds to this point. Of course, the actual site of the arrest is largely dependent upon the actual position of the displaced disc material. The more lateral the obstructing disc fragment, the more lateral the range of arrested circumduction. Unless you have two discs out simultaneously, one on one side and another on the other (this would be unlikely if this is the first episode of severe back pain, but not unusual if you have had several traumatic flexion injuries) your motion should be arrested predominately to one side. If only one piece of disc material is to blame it usually is apparent which side the herniation is on because the pain will be mostly on that same side. As you repeat these diagnostic circumductions alternately clockwise then counterclockwise, the places where your motion is arrested identifies for you the borders of the displaced disc material.
As a procedural consideration, if your pain is predominately right-sided, then start with a clockwise circumduction because that should get you to identify the most anterior aspect of the prolapsed disc first. Then, to locate the other side of the disc bulge you next circumduct in the counterclockwise direction. Keep doing this until you have fixed in your mind the position of the aberrant disc material.
This is much like being given the task of finding the position of a brick placed between two barrels with your eyes closed. You do it simply by progressively rocking the top barrel in a circular/gyrating fashion until you can figure out where the most force is necessary to roll the barrel over the hump that the brick creates. As you “circumduct” the top barrel, the closer the rim gets to the brick, the more energy it takes to force it over the hump. The barrel would be analogous to the barrel-like component of the vertebral bones adjacent to the herniated disc and the herniated disc material would be the brick. I doubt that anyone would have trouble describing the position of a brick between two barrels with their eyes closed, so one needn’t make finding a disc herniation any harder than that. You just have to picture the vertebral bone gyrating above a piece of hard material resting on another similar barrel surface, unmoving below it.
Now, if the disc is herniated directly to the posterior (in the posterior midline) and it is a wide bulge, arrest can occur as early as the 9:00 position circumducting counterclockwise and again at the 3:00 position while circumducting clockwise. This is not unheard of, so when this happens one can assume that the disc bulge is directly in the mid-line, extremely wide based, and herniated directly to the posterior. When this is the case, usually the back pain doesn’t seem to be directed or radiating to one side or the other but stays centrally in the posterior midline or gives pain to both sides more or less equally. In my experience, the centralized disc bulges usually only occur in the lower Lumbar region. I believe this is owing to the extra anatomical strength afforded by the posterior longitudinal ligament as it ascends to the superior reaches of the vertebral column making midline posterior prolapses less likely as one ascends the spinal column. When it enters the lower Lumbar region, the wideness of the vertebral bodies causes the posterior longitudinal ligament to be spread thinner, thus predisposing to posterior midline disc bulging. Also, this area usually sustains the greatest forces when flexion injuries occur, and most people flex directly forward when they lift.
It is so unusual for discs to herniate anteriorly except under extreme traumatic stress such as in an automobile accident or major fall in which the spine is violently hyperextended that I do not feel a discussion of that condition is appropriate here; but if the pain is indicative of an arrest in motion when circumducting through the 9:00 to 12:00 to 3:00 positions, then suspect an anteriorly prolapsed disc.
In the approximately ten years of treating disc herniations, I have seen only a single anterior herniation. Of course, in the event of a major traumatic injury such as mentioned above, an examination by a qualified medical doctor is in order, and an appropriate imaging study might just as easily and safely demonstrate the lesion. Nevertheless, repeated Diagnostic Circumductions around from one side to the other should allow you to fix in your mind the approximate direction and position of the disc bulge.
The level (i.e.: L5-S1, C5-C6, etc.) of the spine where the pain is elicited and at which you should be pivoting tells you the level of the disc segment that is herniated, bulging or prolapsed. For instance, if you lean your torso and center your pivot at the area right where the spine meets the hips and an arrest in motion occurs, your protrusion is probably at the L5-S1 disc space level. If you only need to lean your head to one side and rotate it (as if looking over your shoulder) and the motion is arrested, it is at the C2-C4 level. Depending upon how much you have to lean that portion of your body superior to the area of pain away from the mid-line tells you how far down the putative segment is located. This is understandable because the more away from the midline you have to lean your upper body to get to the painful segment, the lower the portion of the spine that will be required to bend in order to allow for the movement. As that segment bends in the direction of the herniation, bulge or prolapse, the wedge-like, painful sensation is elicited as the bulge is squeezed and the peripheral intervertebral ligaments containing the bulge are stretched.
So, once you have fixed in your mind the borders of the disc bulge as described above, you can carefully aim a leaning extension directly over the center of where the herniation should be. The onset of the pinching, wedge-like, pain (immediately upon the degree of the leaning extension being sufficient to put pressure on it) should confirm the exact center of the disc herniation, bulge, or prolapse. Strictly speaking, when you are compressing the disc directly over its herniation, the pain you feel is mostly due to the hydraulic, direct mechanical, or pincer-like pressure exerted by the displaced disc material pushing against and deforming the posterior component of the capsule (depending upon the displaced disc material’s position relative to the disc’s center). The instant you move off of that point directly over the displaced disc material, the fulcrum pain comes in as adjacent capsular ligaments are stretched.
If there is no arrested motion or pain during this test, either your pain is not due to a disc or you are not leaning far enough off the vertical axis to ideally effect the spinal segment with the herniation. It may sound obvious, but if you are attempting to circumduct by pivoting at the lower Thoracic region, you are probably not going to illicit sufficient discomfort to diagnose a herniation at a low Lumbar lesion and vice versa. To insure such is not the case, you can do some experimental testing by increasing the degree of off-center leaning to find the location of the problematic disc unit.
Diagnostic Circumduction can be used at any level of the spine to determine whether a particular disc is herniated. In the Cervical region, circumducting the head at the neck such that you pivot around the lowest vertebral segment that is painful will give the best determination of the level of the herniated disc material. The Thoracic spine is somewhat more difficult due to its inherent lack of mobility; however cocking the shoulders to effect a leaning gyrating circumduction and focusing your pivotal point slightly below the area of discomfort usually will reveal what segment of the spine is involved. For the Lumbar region, pivoting at the hips usually is enough to confirm where the pain precisely stops your motion. Regardless of the spinal region, the more you increase the angle of the spine superior to the area of concern, the more you activate the disc segment in question. If you keep the spine superior and inferior to the site of pain and the disc unit you are testing relatively straight. That way you can be certain that you are testing only a single disc unit.
You may note, leaning or flexing anteriorly too much towards the opposite side relative to the disc herniation during this test can sometimes elicit a stretching type of pain near the site of the disc herniation because the degree of leaning is so great as to stretch the peripheral intervertebral ligaments affected by the disc herniation or due to the hydraulic-type pressure exerted by a bulging disc material (depending upon the actual type of herniation and degree of off-centered position of the herniation). This means that you are over-doing the degree of anterior flexion or leaning; however, this pain can usually be distinguished from the range of motion, obstructing-type, pain or disc-bulge, pinching, sensation. The pain of too much flexion is more of a stretching type pain and different from the pain induced by trapping and squeezing a herniated piece of disc material that comes while Circumducting in Extension. Also, the stretching type of pain, although brought on by the movements, doesn’t arrest circumduction anteriorly so much as it is so painful that you don’t want to continue to flex forward. Too, straightening up from this pain sometimes produces pain actually greater than the pain you induced by flexion. You should also feel the discomfort on the posterior side opposite to the side towards which you are anteriorly flexing. This is the pain caused by weight-bearing flexion on a herniated disc (to be covered in greater depth later). This is a consequence of the de-centralized disc material being pushed further posteriorly, but I don’t want to confuse the reader anymore by focusing on it, except to say if it occurs, straighten up until it is relieved before it causes the disc to prolapse more and potentially compress a nerve root.
As I indicated above, there are other ligaments, inflamed tendons, and torn or spasmed muscles all possibly present concurrently, any one of which is capable of generating back pain; and, therefore, capable of confusing the picture, especially just after an injury. Since standing and CIRCUMDUCTING while weight-bearing involves the activation of these structures, it can be difficult to distinguish between these sources of pain when trying to determine if de-centralized disc material is the source or if a major contributing component is due to the activation of damaged muscles or tendons. In reality, one can expect these other types of pain, especially spasm, to participate in the total back pain experience especially when in close proximity (both anatomically and near in time) to an injury. In that event, wait a few days or, if necessary, as much as a week or two to let these other structures calm down. They will heal, the disc’s structural tears will not. One can be reasonably certain that if the disc is involved, it will stay broken and eventually it will become apparent that such is the case.
If the Diagnostic Circumduction test described above is not obviously and convincingly successful in distinguishing whether pain is from a piece of decentralized disc material or some other source while weight-bearing, you can try lying down and reproducing the same test in a reclining position. Simply put pillows in such a manner that you can roll or change your position successively to reproduce the same configurations as achieved when leaning and extending from an upright posture. For instance, for the neck area, the obstructive component of the pain can be identified without interference of any other active muscular motions by simply relaxing and propping the head up on a pillow then log-rolling the entire body. In effect, the angle formed by the neck with reference to the axis of the body doesn’t change as the neck is fixed in its orientation and the body moves through space. This moves the selected disc unit through its range of circumduction motion equivalently to the manner which is accomplished while standing only, in this case, it is on a horizontal axis and the body below the disc is doing the moving.
In the reclining scenario, the previously described “O’CONNOR DIAGNOSTIC CIRCUMDUCTION TEST” would be referred to as “PASSIVE” and can be differentiated from the standing test which would be conversely designated as “ACTIVE.” In the upright posture, the body is actively moving and contracting muscles, activating other potentially inflamed soft tissues, and stretching those structures necessary to balance the body; but, in the reclining case, the body is more passively determining the site of the lesion because the disc unit is only moving as a consequence of the body rolling and the non-disc structures are exempted from fighting gravity.
For Thoracic spinal pain, similarly propping the upper torso on pillows or any suitably comfortable structure will suffice. For the Lumbar region, especially while in acute pain, lying on a soft mattress is an excellent vehicle. You will probably be doing that anyway, so you might as well “make hay while the sun shines.” As the body sinks into the mattress while a pillow or the elbows raise the prone torso up, the Lumbar spine passively assumes an extended posture. Rolling through the same pattern as above can reveal the same information. Instead of leaning and gyrating, you only need to roll from side to side to localize the site of the de-centralized disc material. The principle is the same, only the passive positioning eliminates the likelihood that spasm and inflamed tendons or muscles are being activated to cause the pain.
After becoming very familiar with these methods, through repeated experience, the reader can expect to instantly identify when the disc material has become de-centralized and instigating the pain from any position. Once familiar with the feeling (especially if your disc material repeatedly is prone to de-centralization), every time it goes “out” you can immediately tell if it is “out” by gently circumducting from even a seated position. It isn’t necessary to make a big project out of circumducting after you conceptualize the mechanics and become adept at the movement. After a while, simply rolling the neck or shoulders around from almost any position will reveal the presence and position of Cervical or Thoracic decentralized material, and gyrating the hips without so much as changing your seated position can be expected, eventually, to be all that is required for the “expert” you can become at your own back pain diagnosis.
I’ve become so adept at doing it, when I suspect (due to the onset of discomfort) the disc material has migrated, I only need to lean towards the place where it usually displaces and feel the characteristic “wedge-like” pain to confirm whether it is truly “out” or not. I don’t necessarily have to go through the entire Diagnostic Circumduction process I described above. Don’t think that just because I described it in such exacting detail that you need to obsessively adhere to the entire rigmarole forever. Even while driving, I can shift my hips in a leaning posture and feel the “wedge” or “lump.” I then can do the appropriate maneuver (to be described later) and relieve the pain. There is no reason why anyone else who comprehends the mechanical principle of this test cannot do likewise. Reading on, the maneuver will be taught so that once the displaced disc material is identified, it can be re-centralized with equal ease.
In the absence of Diagnostic Circumductional Arrest throughout the full range of posterior extension, it is harder to evoke a decentralized disc as the origin of the pain. If nothing stops or limits you when making these gyratory movements, the pain is possibly not from herniated, protruding, or de-centralized disc material’s effect upon the capsular intervertebral ligaments and the re-centralizing maneuvers described later will have a lower probability of helping your type of back pain. However, I have known patients who involuntarily splint the affected segment and despite attempts to circumduct at the affected segment; instead, unconsciously they circumduct only at the segments above or below it. Therefore, simply because you do not get a pain that arrests your movement does not mean that the maneuvers outlined in this book will not help you. I have had several patients who are helped by my method yet never had an arrested motion that I could identify. In one case, I was able to conclude that the person was so flexible and had accommodated to the pain for so long that other segments of the spine performed all the circumductatory movements without necessitating the activation of the involved segment or she was so accustomed to the pain that she unconsciously avoided the use of that segment. The maneuvers worked very well in this patient, ending her years of neck pain.
Consequently, I would suggest that the readers attempt the maneuvers described later in the book, regardless of whether or not they have a rotational Circumduction Arrest or if they understand how to diagnose their own disc. Anyone with back pain has nothing to lose and everything to gain by trying The O’Connor Technique™ maneuvers. Sometimes, when I see that patients are not arresting in their own circumduction attempts even though I have instructed them in what to do, I can usually properly guide their movements so as to insure that the affected segment is being loaded or stressed. This usually proves to me that, indeed, they have an arresting component due to a disc problem; and I can locate it even though they cannot without physical, individualized, and personal guidance. However, it is impossible for me to examine every one of this book’s readers who have herniations but are unable to properly perform a Diagnostic Circumduction. This series of movements is designed so that you can do it yourself; and, thereby, identify the site, direction, and position of the displaced disc material. If that cannot be accomplished, no big deal, continue reading; and, after the method becomes known to you, you can come back and try it again to see if you can succeed. In other words, don’t get frustrated, disappointed, or give up just yet because the foregoing appears to be too complex or difficult.
Of note here, even though I’m getting ahead of myself, when the maneuvers described later in the book are successfully accomplished, one can expect this “wedge”-like pain that arrests your movement and the obstructive component of the pain to be instantly resolved. As the disc material is re-centralized, it no longer impedes the normal circumductatory and gyrational actions of the spine. When the displaced disc material goes back into its central location, it does so usually with dramatic relief because it no longer obstructs the normal circumductatory capacity of the spine. If the maneuvers are accomplished and no dramatic relief is achieved, then probably either a disc is not the problem or the corrective maneuvers are not being accomplished properly and, therefore, not yet successful in replacing the misplaced disc material.
Repeating this “test” but treating it as a component of a maneuver while unweighting the superior part of the body above the lesion at the end of one of the maneuvers that are described later in this book also can re-seat a displaced disc that is not very much off-center. I often see people with mild back symptoms performing this type of movement (especially after getting out and stretching after long drives) because it gives those with minimally displaced disc material relief from the “stiffness” they experience due to the prolonged Weight-Bearing Flexion of driving.
Often, the maneuvers I describe later in the book are able to move the disc material almost completely, but a little extra nudge is necessary to get them to seat completely. Simply doing a mild weight-bearing Therapeutic Circumduction nearly identical to the “O’Connor Test” frequently accomplishes the “coup-de-Grace” and provides the final effort necessary to completely re-seat the disc, but more about this aspect later.
Another reasonable rule of thumb to be guided by is that, if there is no arrested motion on weight-bearing Diagnostic Circumduction, the disc material (or fragments of same) are probably not decentralized. An interesting problem sometimes prevents the immediately successful resolution of all components of the back pain. The disc material can have been returned to the proper centralized position, yet a residual pain may still be present. When it seems that even though you are doing everything as you are supposed to do and recreating the same sequences of maneuvers (as will be described later) that were successful in the past, yet still nothing seems to totally stop the residual pain, it often is the case that the disc fragment has been putting pressure on the capsule’s ligaments so long that an inflammatory focus has been created. In this case, there may be pain associated with flexion or extension; yet no actual arrested motion.
In that event, using anti-inflammatory medications and rest to prevent repetitive irritation of the inflammatory focus is the best policy to relieve residual pain. More on that subject follows later in the section on medicines and strategy for pain relief; but inflammatory pain is of a dull aching or warm (like heat generating) character, continuous, and present regardless of the position. Then, it probably originates from an arthritis-like inflammation of the joints, ligaments, or tendons acting on some nearby spinal segments. Especially, the accessory articulations of the vertebral bones (the facet joints) can also become inflamed. Facet pain is usually distinguishable from the pain of a herniated disc because facet joint arthritis pain has no physically arresting component, hurts when standing, and relieved by sitting (the opposite of disc pain.) In this case, drugs like acetaminophen, aspirin, Ibuprofen (Advil, Motrin, Nuprin, etc.) or other non-steroidal anti-inflammatory drugs are indicated. These drugs are often helpful for pain of disc origin, also; but, usually, they don’t offer much relief if the disc material is still “out.” After the disc has been re-centralized, the anti-inflammatory medicines are especially helpful in reducing the pain caused by the disc material rubbing against the ligaments or the inflammatory arthritic pain caused by the vertebral bodies rubbing together when discs degenerate to the point that the disc space has collapsed.
The key to this consideration, of course, is the understanding that if the disc is decentralized, the “wedge”-like pain that stops your movement will be present while leaning and Circumducting in Extension. If you have completed a successful maneuver that frees up the circumductatory capacity of the involved spinal segment such that there is no longer the arrest in Diagnostic Circumduction that there was before completing the maneuver yet there still is pain coming from that area, this is probably a residual soreness or inflammatory-type pain. Understandably, if a disc has been protruding and tearing the adjacent ligamentous structures, they will have been damaged or at least irritated. Be aware that once an inflammatory focus is set up after prolonged pressure due to protruding disc material, it is reasonable to assume it will take some time and anti-inflammatory medication to achieve total relief.
Many times, I have “fixed” a person’s back to the extent that they no longer have arrested motion; but they continue to describe pain for a short time afterwards. Usually, the pain is of such reduced severity and so closely related to the maneuver done to them that they acknowledge the relief came from my method. Most patients recognize that the majority of the pain is gone the following day, attributing my application of The O’Connor Technique™ as the point when their recovery began.
DOCUMENTING YOUR DISC

Figure 5; Posterior view of back with spine superimposed.
Back pain episodes are frequently separated by long intervals between painful events. For that reason, it is easy to forget the site of the displaced disc material or, more importantly, the particular maneuver or sequence of movements that successfully alleviated that unique pain. So as to give your back its best chance for the earliest recovery, take notes to document the major components of the pain. By identifying the areas of pain for future reference, any particular pain pattern can be reasonably assumed to be originating from the same disc in the same position when it recurs. Therefore, if a particular site is identified and a unique maneuver (the maneuvers are to be described later) is successful, you can document both the level and direction of the displaced material as well as the movements that were most successful in alleviating that pain. Then, when an identical pain recurs at some time in the distant future, that maneuver or sequence can be immediately employed to occasion relief without relying solely on the memory or trial-and-error.
It is best to characterize the pain in a systematic fashion. First, locate it by level of the spine where the pain is greatest. Certainly, you wouldn’t be expected to be successful doing the same corrective maneuver for a problem centered at the high Thoracic level on the left that you would do for a pain originating at the Low Lumbar region on the right. So, it makes sense to keep track of where the problem is physically located so that the proper maneuver can be chosen later. Next, on a diagram like the one provided here (Figure 5), cross hatch the exact region (level) of the particular spinal pain where it seems to be centered and to where it radiates. Note where the sharpest pain is the most severe and any movements or positions which increase the pain.
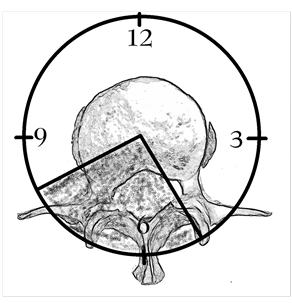
Figure 6; “Pie Chart” superimposed upon a disc showing arrested range of motion area.
After that, on a view that looks down upon the disc, draw a triangular “piece of pie” over the area which brings on the sharp pain during the Diagnostic Circumductional motions described above in “SELF-DIAGNOSING YOUR DISC“. It matters little whether you choose a format like a clock or a 360 degree circle to diagram the wedge shaped area of arrested motion so long as it is in some way recognized, understood, and documented. I find it advantageous to draw a diagram like a pie chart so that the areas with pain-free range of motion are distinguished from the areas where range of motion is arrested and pain is elicited (Figure 6).
Keeping such documentation helps to recall the exact location of the de-centralized disc material so one needn’t repeat the testing every time. You will appreciate the necessity for documenting or fixing in your mind the exact location of the displaced disc material, later, as the maneuvers are described because you will also (later in the book) be asked to document the exact maneuver that gets you out of pain; and you will want to reference a particular drawing to a particular maneuver. The diagrams provided in this book (Figures 3 and 5) can be copied and drawn on to serve that purpose. Like writing down the description and combination to a safe, this becomes especially helpful and necessary if you have multi-level disc problems or if the disc is particularly difficult to re-centralize.
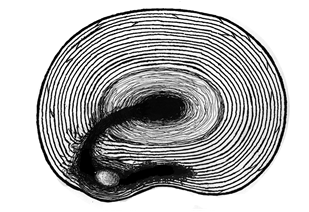
Figure 7; Disc material trapped between layers of annulus fibrosus.
Documentation becomes especially important whenever there are complex cases in which the pain appears to move from side to midline, side to side, or from midline to the side during a Weighted Circumductional movement. This can mean that you have a mobile piece of disc material moving laterally through a concentric tear or a piece of disc material moving within a space between the laminations of the annulus fibrosus or between the capsule (the ligamentous peripheral layer of the disc) and the annulus fibrosus (as portrayed in Figure 7).
In that event, a recollection of where the original pain started and where it went to during any particular maneuver may give a clue as to the location of the disc material. Sometimes such a method can elaborate the original tract through which the disc material traveled. The eventual goal is, then, to design or describe a means by which you can work the material back to the center of the disc as though you were playing a “BB in a maze” game.
If the degree of disc degeneration is extensive and the product of multiple traumatic events the goal becomes not highly unlike moving a BB through a circular type maze game. In order to get the BB to the center you have to move the BB centrally at precisely the right instant where a gap in the walls will allow its movement to proceed centrally. In order to get to that gap, the BB has to be caused to move circumferentially by progressive application of forces directed to allow its movement to proceed in the ideal direction. In this analogy, the walls of the maze are the laminar array of the fractured annulus fibrosus laminations contained within the intervertebral capsule ligaments and the BB is the solidified central disc material that once was the liquid nucleus pulposus. Unfortunately, you cannot see the BB to know when it is in the ideal position to move centrally. This causes you to rely upon trial and error. When you are successful, it probably is in your best interests to document what you did to succeed so as to reproduce that same series of movements the next time.
This is a potentially important distinction to be made and documented because if one has a disc like that seen in Figure 7, a Diagnostic Circumduction in a counter clockwise direction can result in the pain changing from the left posterior to the right posterior. You should take note of this type of reaction when documenting your disc pain. The significance of this will become apparent in later reading on maneuvers.
Don’t get frustrated by reading this because of its apparent complexity and not knowing yet what constitutes a maneuver. Statistically speaking, you probably don’t have a disc of this configuration; but, if you do, and the simple efforts don’t seem to work, you may have to resort to a more complex strategy. In that case, the first effort would be made to return the disc fragment to the site where the pain originated, then find the tract through which it traveled so it can be moved back to the center. This may require a gentle weight-bearing circumductional movement before an unweighted flexion in a certain position then followed by a directed extension. Specifically writing down the exact sequence of movements correlated with the disc map and paying particular attention to the successful positions that ultimately result in the relief of pain can save hours of ineffective movements being repeated if and when your back goes “out” again.
Even though I’m getting ahead of myself by discussing maneuvers, the nature of which are still obscure to the reader who has not yet read Chapter 5, a discussion describing documentation of a “puzzle” would not be complete without including a recommendation to retain in writing the solution to the puzzle, or if you will, the combination to your “safe”. In summary, it is important to take a few notes to describe both the pain pattern and the directions for the ideal maneuver that gets you out of that particular pain pattern. Later, as you are exposed to the maneuvers, the necessity for this consideration and the means to accomplish it will become obvious.
1. Leblan K, et al. Report of the Quebec task force on spinal disorders. Spine. 1987;12:S1-S8.
2. Op.Cit. Chapter One, Endnote #2;AHCRP publication 95-0643.
3. Helms CA, Pearson DO, Neck and Spine, Patient Care, (1996) Sept. 30: 55-74
4. Sward L, Hellstrom M, Jacobsson B, et al, Gothenburg University, Gothenburg, Sweden, and King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia. Back pain and radiologic changes in the thoraco-lumbar spine of athletes, Spine. Feb 1990;15:124-129.
5. Deyo R, Diehl AK, quoted in Lower Back Pain: When do you order X-Rays?, Emergency Medicine; October 30, 1989:63-66.
6. Bowden SD, Davis DO, Dina TS, et al. Abnormal magnetic resonance scans of lumbar spine in asymptomatic subjects. J Bone Joint Surg. 1990; 72:403.