CHAPTER TWO: PHYSICAL REALITY
SPINAL ANATOMY
In order to comprehend the concepts presented in this book it is essential to acquire a clear understanding of the vertebral column’s basic anatomy. Since this book is not intended to be an all-encompassing re-creation of the great anatomical textbooks, I have chosen to limit discussion to only those anatomical terms and features that have a direct bearing upon the understanding of The O’Connor Technique™. For a more extensive elaboration of spinal features, the reader is directed to any medical school anatomy textbook by which they choose to be bored.
Don’t be intimidated by a few new terms. It takes only a few minutes to quickly learn them and be able to employ them in the context of the ensuing discussions. I have intentionally limited the technical aspects of the book to a minimum because it is more important that the layman understands what is going on than for me to be able to market this book as the definitive reference on the spine to my physician colleagues. If, at first, it is hard to keep the terms straight, just refer to the diagrams every time you need to refresh your mind as you read on. I have made a distinct effort to repeat and clarify whenever technical terms are used that aren’t readily known by most people. So, don’t get bogged down trying to memorize all the names of the body parts because you erroneously believe that you must commit them to memory before you can understand the remainder of the book. Keep reading, look at the diagrams, and refer back to the definitions whenever you are not certain about a particular term or technical name.
Unfortunately, unique things have unique names and to understand a novel topic, you must be prepared to learn a few new words. Referring to a particular anatomical structure as “the little thing in the back,” would only denigrate the accuracy of what is presented here and make things more confusing. So, just don’t look upon it as a burden, and settle in to learn a few new words if you already don’t know them. Assuming that the reader is not immediately technically oriented, I have made an effort to repeat the definitions in the text so that as it is read, the positional anatomy is clarified until the reader is sufficiently familiar with the terms.
DIRECTIONAL TERMINOLOGY
The following terms are frequently used in medical terminology to describe anatomical directions. They can be used to describe the entire body or any of its parts. One should have a familiarity with them in order to fully understand the concepts, positions, and movements described throughout the book:
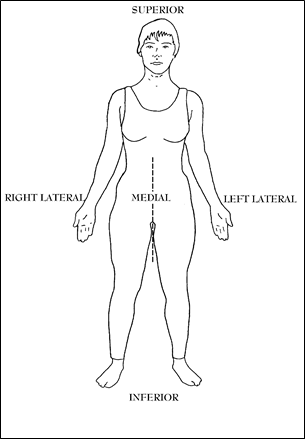
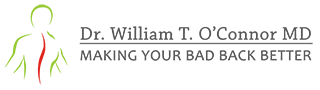
Figure 1; Anatomical terms.
SUPERIOR–means in the direction of the top of the head or the top of the body. Saying “up” is often inaccurate because if a person is lying on their back, “up” is really anterior, so using the term “superior” is superior because it is always references towards the head’s aspect of the anatomical part in question. The whole body or any part can be moved superiorly if it moves in the direction of the head.
INFERIOR–means in the direction of the soles of the feet and situated below or directed downward. It can also refer to that part of the body or body part closest to the feet (such as “the inferior aspect of the chin”). The whole body can be moved inferiorly if it moves in the direction of the feet.
LATERAL–refers to the sides of the body. There is a left and right lateral (side) aspect to just about every anatomical part as well as the body in general. When the term lateral aspect is used it refers to that component of anatomy away from the midline of the trunk. When something moves laterally, it moves away from the midline.
MEDIAL–refers to the center or midline of the body or body part. When an anatomical structure is said to be medial, it is more towards the midline of the torso. Often, the term, medial aspect, is used and that refers to that component of anatomy closest to the midline of the trunk. Something moves medially if it moves towards the midline.
ANTERIOR–means toward the front of the body. One can move a body part anteriorly by moving it towards the front of the body. A body part can have an anterior aspect, that being that component closest to the front of the body. From the word “ante” which refers to something “up front,” before, or at the beginning, such as in antebellum (before the Civil War) or like what you do before you play a hand of “penny-“ante” poker. You put up a penny up front as a bet.
POSTERIOR–means toward the back surface or rear of the body, such as getting kicked in your “posterior.” It can reference a part of the body in relation to another such as the vertebral bone parts that are closest to the back surface of the body are referred to as the posterior elements. One can also move a body part to the posterior by moving it towards the back surface of the body.
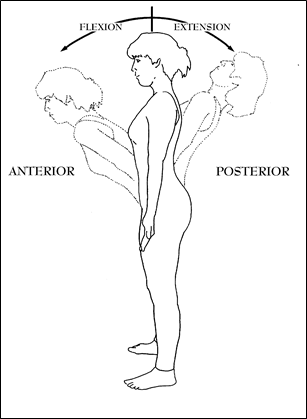
Figure 2; Flexion and Extension at the Lumbar region from the Neutral anatomical position.
FLEXION–from “to bend” in Latin. Any time you decrease the angle made by two bones you “flex” at the joint which joins those two bones. In the case of the spine, bending forward produces the action of anterior flexion when viewed from the side. When viewed from the front, a person can bend to the side and the spine can be said to laterally flex or bend. Spinal Flexion in this book refers to any movement that bends the spine anteriorly whether the spine is in the neutral position or while in an extended posture flexes to return towards the neutral position.
EXTENSION–the opposite of flexion, from the Latin for “stretching out” and therefore is an increase in the angle formed by the axis of two bones. This can refer to the body being brought back to the neutral, resting, anatomical position from a flexed position, or going from the neutral anatomical position towards the posterior.
Figure 3; Circumduction at the Lumbar region.
If a person bends backwards or posteriorly, the spine is said to perform extension, regardless of any other position the body may be assuming at the same time. The spine can be in flexion and extend to the neutral position or be in the neutral position and extend to the posterior. Also, the spine can be in extension and extend maximally beyond the usual range of motion into hyperextension.
CIRCUMDUCTION–from the Latin “to draw around.” This is actually a combination of the movements previously described. It consists of a smooth series of movements (Shown in Figure 3) starting with anterior flexion, leaning into lateral flexion, lateral extension, and posterior extension in that specific sequence. In this example, the circumduction takes the upper body in a clockwise direction. However, it could start at any point on the circle, go only part way around, or even go in the opposite direction; and it still would be considered circumduction. If this action is performed at any level of the spine, the portion of the body above the point of movement will be brought anteriorly and laterally, then posteriorly and then medially, resulting in the superior aspect of the anatomy to gyrate around in a circular pattern. Since the inferior aspect of the spine below the point of motion is fixed in this example, the upper section moves through its range of motion carving out the form of an inverted cone in space.
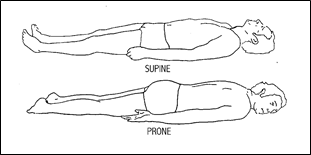
Figure 4; Prone and supine position.
SUPINE–that position in which a person lies flat with the face, abdomen, and toes pointing up.
PRONE–that position in which a person lies flat with the face, abdomen, and toes all pointing down.
STRUCTURAL ANATOMY
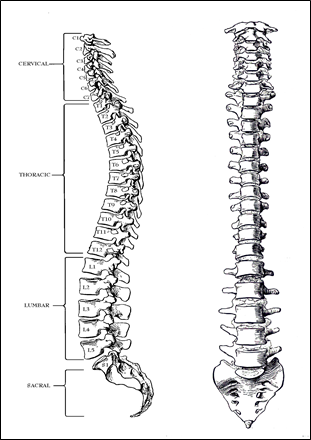
Figure 5; Vertebral Column.
The spinal column has classically been divided into several structurally and functionally distinct sections, the cervical spine, the thoracic spine, the lumbar spine and the sacral spine. Largely, this book deals with the cervical, thoracic, and lumbar sections since the sacral section is functionally fused and offers little opportunity for mechanical manipulation except where it interfaces with the lumbar spine at L-5, which is probably the most problematic area in the spine because it is the first mobile segment above the rigid pelvis. (See Figure 5)
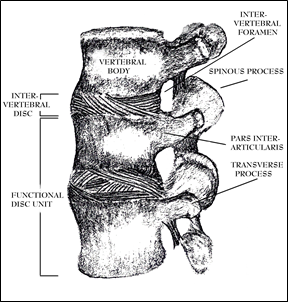
Figure 6; Vertebral Column Segment L3-L5.
It is important here to note the curvature of the spine. It is not a straight linear structure when viewed from the side (or the “lateral” view). The major curves are seen at the cervical and lumbar regions where the majority of flexibility is also present.
One can look upon the spinal column as an incredibly strong central support structure upon which the trunk and upper body rest similar to a long series of bony spools separated by cushions. The spools being named the vertebral bodies and the cushions are the intervertebral discs (or simply referred to as the “disc”). A functional disc unit is comprised of the vertebral bone above and below an interposed disc (see Fig. 6).
The anterior portion of the vertebral column (spools with cushions between them) is a weight bearing, shock absorbing, flexible structure capable of amazing feats of strength. The posterior portion is composed of bony bridges and spikes that protect the spinal cord and nerves, acts both as a moment arm and as a fulcrum, and guides the movement of the functional unit while maintaining the vertebral bones’ positions relative to the each other. As can be seen in Figure 7, the anterior and posterior components join at the pars interarticularis to create a canal through which the spinal cord travels and sends its major branches, the spinal nerves, out through spaces called intervertebral foramens. The superior aspect of the intervertebral foramen is composed of one pars interarticularis and the inferior border is composed of the vertebral bone adjacent and inferior to it.
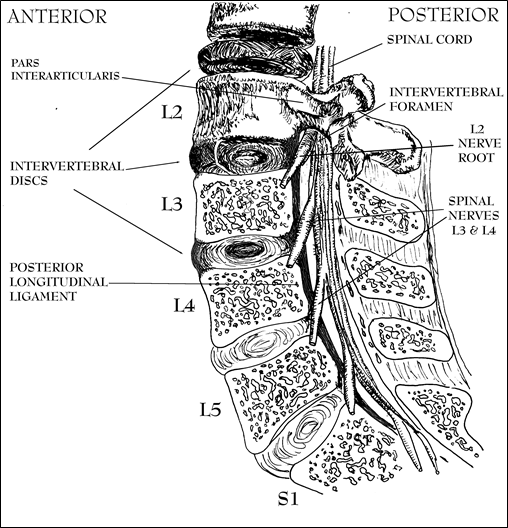
Figure 7; Cut-away lateral view of Lumbar Spine.
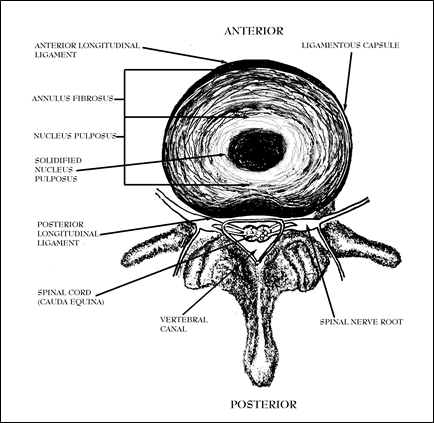
Figure 8; Cross-section of Intervertebral Disc from above looking down.
A view looking down on a cross-section of the vertebral bones can be seen in Figure 8 so the reader can understand the relationships between these structures. Especially important is the close proximity of the discs to the spinal nerves. If a disc ruptures posteriorly, it can be easily seen to be capable of impinging upon a spinal nerve root and damaging it, resulting in paralysis and anesthesia.
For the purposes of this book, the posterior elements can be largely ignored. Not that they do not serve as sources of pain such as arthritis (because they contain joints) or sprains (because they have ligaments holding them together); but, in the largest part, the mechanical pain experienced in the spine originates from a degeneration of the stress-dissipating and pressure containment structures known as the intervertebral discs.
Of course, the intervertebral disc (usually referred to simply as the “disc”) is not the only structure that dissipates stresses placed on the spine. With flexion, extension, rotation, or shear stress, the load distribution on the entire functional unit is shared by the intervertebral disc, anterior and posterior longitudinal ligaments, the facet joints and the capsule, and other ligamentous structures like the ligamentum flavum and the interspinous and supra spinous ligaments, which attach to the posterior elements of the functional unit. Those anatomical structures other than those directly contiguous with the disc are largely unamenable to mechanical manipulation and don’t usually get into trouble without major trauma (by major trauma, I refer to falls off of roofs or major motor vehicle accidents as opposed to minor trauma like lifting garbage cans); therefore, they are outside of the scope of this book. They need not be focused upon in this book because to do so would just be confusing and distract the reader from the major goal of understanding that the most common source of a “bad back” is damage to the disc itself. However, that is not to say that the other problematic entities are insignificant or incapable of producing misery, it is just that the other causes of back pain are both individually and cumulatively in the distinct minority. In fact, if one doesn’t achieve relief from practicing the principles of The O’Connor Technique™, it is unlikely that a disc is the source of the pain; and I would encourage that category of patient to seek help elsewhere armed with the reassurance that they have probably eliminated disc disease as the origin of their pain.
The spool-like vertebral bodies are held together with tough ligaments that connect bone to bone. On the front (anterior) surfaces lie the anterior longitudinal ligaments and at the back (posterior) surfaces lie the posterior longitudinal ligaments. These two major ligament systems which traverse the spine lengthwise blend at the disc spaces between vertebral bodies with other laterally situated, ligamentous structures of the spine (the lateral intervertebral ligaments) that also run longitudinally along the axis of the spinal column. All these ligaments merge together to circumferentially enclose the more cartilage-like central regions of the disc, forming what is often referred to as a “capsule” at the disc level. This capsule consists of dense, strong fibers that are firmly bound to each adjacent vertebral body. These sheets of ligamentous material blend with the peripheral, most dense, portion of the annulus fibrosus and function to contain both the more gelatinous inner sections of the annulus fibrosus and, in turn, the more liquid nucleus pulposus (See Figures 8 & 9).
This ligamentous capsule, in combination with the concave shapes of the vertebral bones’ surfaces, keeps the more internal components of disc material positioned in line with and centrally between the vertebral bodies of the spine. When the body bends forward (flexes), the postero-lateral ligamentous lamina (layers) and the posterior longitudinal ligaments straighten, tighten, and assume a more linear axis, preventing the posterior aspects of the vertebrae from totally separating or coming apart while retaining flexibility. The anterior ligaments perform likewise for the anterior when one bends posteriorly (extends).
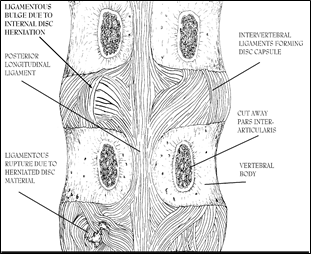
Figure 9; Posterior view of vertebral ligaments with pars interarticularis cut away.
Other ligaments which are attached to the processes of the vertebral bodies also function to hold the entire apparatus together; however, they are not as pertinent to the principles of this book because the posterior longitudinal and the intervertebral capsules’ ligamentous structures are the fibers which house and keep the cartilaginous disc material from moving posteriorly. Were it not for these ligaments, the discs would have no structural elements to maintain the central disc material positioned correctly between the vertebral bodies. Figure 9 shows these ligaments with their normal structure on the right and their damaged structure on the left. When these structures are damaged, they no longer prevent the central disc material from moving posteriorly, the profound significance of which will become apparent later.
The ligamentous tissues that form the disc’s capsule are well-supplied by nerves– both stretch and pain receptors. This nerve supply enables the brain to know where in space (relative to the other bones) a given bone is positioned, enabling a human to stand erect and balance the portion of the body above the hips with his spine. In contrast to the outer, peripheral, ligamentous structures, the material deep to the capsule, the annulus fibrosus and the nucleus pulposus, do not have a nerve supply (See Figure 10). So, disc pain, when it is present, comes from structures other than the more liquid “cushions” or any other structures deeper than a few millimeters from the surface of the disc. This fact leads some to conclude the common misconception that a patient cannot have pain from their discs. On the contrary, when the disc material that should remain secure within the center presses upon or distorts the ligaments that surround the disc, the pain can be exceptionally intense.
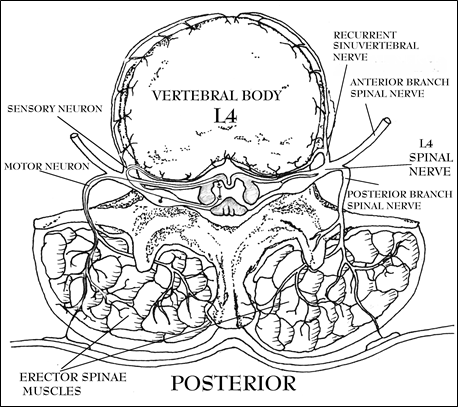
Figure 10; Nerve supply to disc and muscles.
More on pain later; but, for now, it is helpful to understand that the numbered spinal nerves exit the spinal column at the level of the disc inferior to the same numbered vertebral bone. So, the Second Lumbar (L2) nerve and its root (See Figure 7) passes out of the spinal column at the level of the disc below the Second Lumbar Vertebrae through the intervertebral foramen partly formed by the inferior component of its pars interarticularis (also known as a pedicle). The intervertebral foramens are round spaces (between one pars interarticularis and the next) created by the spinal bones through which pass the spinal nerve roots (See Figures 6&8). The spinal nerves supply motor and sensory functions to their corresponding segments of the body. The proximity of these structures to the intervertebral disc is important because if the central disc material herniates and protrudes it can irritate or trap the spinal nerves resulting in pain, loss of sensation, and/or paralysis wherever the effected nerve roots supply innervation. The pattern of this pain is classically described in terms of what structures are supplied by the nerves: dermatomes (areas of skin), myotomes (muscles), sclerotomes (bones, joints, & ligaments) to which the individual nerves for each major spinal nerve travel.
It is technically interesting to know what each spinal nerve innervates so that when pain is felt or function lost it can be localized to a particular spinal nerve and, hence, a doctor can determine which disc protrusion is compressing its corresponding nerve. Such detail is too complex for the intended readers of this book. The reader is free to research any of a number of medical textbooks for this additional information; however I have found this level of expertise confusing and unnecessary to understand the concepts of The O’Connor Technique™.
What is important to understand is that each numbered spinal nerve sends a branch (the recurrent sinuvertebral nerve) to the ligaments that surround and contain the disc immediately inferior to the same numbered vertebral bone. The pain and sensory fibers of the discs travel in these nerve branches (See Figure 10). The recurrent sinuvertebral nerve is significant because if pain comes from a disc’s ligamentous capsule it travels in that nerve. Pain impulses from this nerve can be interpreted by the brain as coming from the larger, numbered, spinal nerve in which it travels as one of many other different nerves. The implications of this anatomical design peculiarity will become more apparent later, but suffice it to say, here, that this phenomenon can explain why pain in the disc can masquerade as pain in the extremities and why muscles distant from the actual site of disc pain can go into spasm even though the muscle itself has not been actually traumatized. More on this subject when pain is discussed.
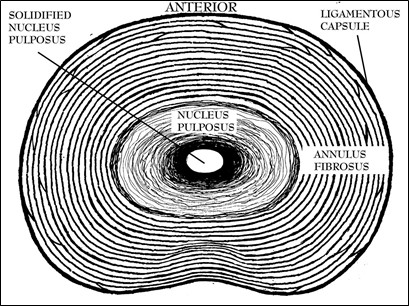
Figure 11; Cross-sectional view of Intervertebral disc viewed from superior.
It is very pertinent to the understanding of The O’Connor Technique™ to have a view of the disc in the mind’s eye. The intervertebral discs’ spherical centers are composed of a gelatinous liquid cartilage material identified as the nucleus pulposus surrounded by an intermeshing laminated concentric fibrous structure known as the annulus fibrosus. The annulus fibrosus is designed with fibrocartilaginous and fibrous protein tissue arranged in concentric layers, each of which attach one vertebrae to the other (See Figure 11). As one moves, anatomically speaking, from the nucleus pulposus to the periphery, the tissues become denser, stronger, less elastic, less fluid, and more ligamentous until reaching the outermost layers. There, the tissues actually become a tough, capsular ligament.
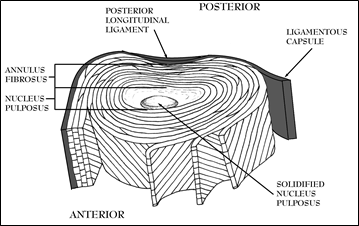
Figure 12; Intervertebral Disc Laminations.
The laminations of the annulus fibrosus are arranged in bands of tough elastic tissue whose fibers run at oblique angles to the adjacent layers to form a shock absorber (See Figure 12), built like a gelatinous/liquid surrounded by layers of Chinese finger traps. As vertically (axial) directed forces are placed upon a disc’s liquid center (nucleus pulposus) it deforms by flattening along a horizontal plane. In this way, the pressure is absorbed and contained by the laminations of the annulus fibrosus. The fibers of the annulus fibrosus are firmly secured to the vertebral bones and mingle with the lateral ligamentous structures as well as the anterior and posterior longitudinal ligaments.
To experience an accurate representation of this structure’s consistency, the reader can go to a meat market that stocks large ox tails. Feeling with a finger the center portion of the largest ones and, often in older animal’s discs, you can appreciate the liquid character and the central hardened material by pressing the center of the circular white solidified segment. A nearly identical structural design is located in the human disc. By manipulating the hard center structure, one can appreciate how it can be moved with alterations in pressure supplied by the finger. When one bends the spine, forces are placed upon the disc that cause the part-liquid/part-solid, disc material to be equivalently moved.
FUNCTIONAL ANATOMY
The nucleus pulposus in combination with the annulus fibrosus affords shock absorbency function to the disc and allows the functional disc unit its dynamic flexibility. With compressive forces, the nucleus pulposus stretches the annular fibers somewhat like a jelly filled tennis ball would flatten when a weight was placed on it. Flexion or extension of the functional unit occurs in part because of the horizontal shift of fluid within the disc, resulting in the expansion of the annular fibers posteriorly or anteriorly, respectively. The elastic nature of the annular fibers tend to oppose and contain the movement of the nucleus pulposus, thereby, tending to restore the functional disc unit to its resting state when the compressive forces are relieved. Sadly, as the disc ages, this elasticity is gradually lost and the capability of the disc to recoil from compressive forces decreases.
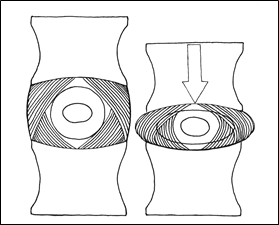
Figure 13; Disc as Shock Absorber.
Fibro-cartilaginous structures like those comprising the annulus fibrosus have some measure of elasticity; but their fibers are largely fixed in their maximum length and, if stretched beyond that, especially if done rapidly, they can fracture or fragment. When these types of tissues tear or break, they (as a rule after childhood) do not repair themselves. Even the peripheral ligamentous structures do not heal by re-making equivalent tissue (as is often incorrectly assumed) but are replaced by scar. Unfortunately, the scar tissue is never quite as strong as the previously intact ligament. The ramifications of this fact will become painfully apparent as an understanding of disc “disease” unfolds later.
Thus, the combination of the annulus fibrosus and the ligamentous capsular structures surrounding it functions to contain the shock absorbing, weight-bearing, liquid center, yet at the same time, allowing an incredible amount of flexibility. If one wishes to appreciate just how flexible, dynamic, adaptable, and amazing a structure the homo sapiens vertebral column is, just watch an Olympic gymnastics competition and compare the flexibility seen there with the strength displayed in the weight-lifting sessions. For all its supposed faults, the vertebral column still garners an awesome depth of respect from this author.
The intact spine is no anatomical or physiological wimp by any stretch of the imagination. The lower lumbar discs can sustain loads of 1,000 Kilograms (2,200 lbs) when stressed with pure compressive forces. In a rather narrow-visioned perspective, many “experts” criticize the evolutionary design of the back by asserting that the vertebral column has not adequately developed evolutionarily to support man’s upright posture. I would argue that it is doing a fantastic job, and a more adequate structure-for-function relationship doesn’t exist within the parameters of biological design.
Thinking about it from an evolutionary survival standpoint, humans do not really need their back after they have reproduced and successfully raised their children to the age when they can fend for themselves. That’s just about the time the discs start to age and break down. I think Evolution and/or God designed it pretty well considering what it is capable of accomplishing. It is only when humans are no longer useful (from a Darwinian perspective) does the spine fail.
Reportedly, aboriginally-living peoples experience a much lower prevalence of disc disease. The peaceful, archetypal, hunter-gatherers infrequently need put the forces on the spine sufficient to herniate discs. Only when man socially “evolves” to the level wherein he routinely builds structures out of heavy materials, fights one another, eats so much excess food that he becomes twice the weight he was designed to accommodate, or performs feats of athletic largess beyond the limits for which it was intended, does he destroy the integrity his spine. Our problem is not inferior spinal construction, the design is perfect for “Gardening in Eden.” Our problem is that the evolution of our tools and their use has not caught up with the design specifications imposed by an otherwise perfectly suited creation. Thus far, unable to find “the right tool for the right job,” we have resorted to using our backs as tools–mostly in pursuit of purposes for which they were not constructed to accommodate. One can hardly charge Nature with the sin of imperfection when it is our own chosen misgivings at fault.
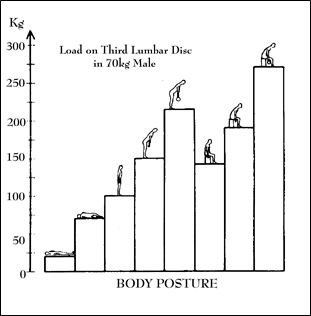
Figure 14; Disc Loads in various postures (From Nachemson, Acta Orthop Scand, 36:425, 1965).
This point is exemplified, and the reader can gain an appreciation of the magnitude of the forces applied to the disc, by an enterprising researcher who once convinced a number of average-sized study subjects (70 kg male volunteers) to allow him to stick needles in their intervertebral discs. He attached the needles to a pressure measuring device and put the people in varying positions. He found that the load on the lumbar disc varied from between 25 kilograms (55 lbs) when lying down to over 250 kilograms (550 lbs) in the seated, forward bending position. (Figure 14)
Interestingly, simply sitting generated load magnitudes equal to standing stooped forward in moderate flexion (about 150 kg). Sitting with the back in flexion was worse, generating about 180 kg of load force. The greatest load was experienced when the subjects held a weight while seated and flexed. This position developed disc loads in excess of 275 kg.–that’s over 600 pounds of force! This explains why even the simple task of lifting a garbage can may result in putting your back “out” as well as why driving occupations carry such a high risk for disc disease. When driving, one is essentially sitting in a forward flexed position while the bumps and vibration of the road intermittently magnify the stresses at high frequency.
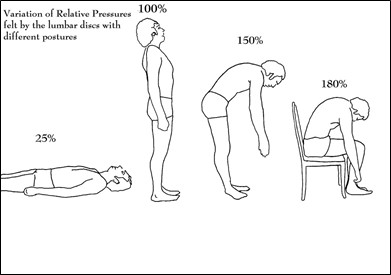
Figure 15; Disc pressures represented as a percentage of standing pressure.
When these numbers are expressed as percentages of the pressure experienced at the disc while standing (See Figure 15), one can see that the simple act of flexion increases the hydraulic pressure of the disc by fifty percent. Sitting and flexing increases it to one hundred and eighty percent. The significance of these pressures and their increases with flexion will become manifest later when this pressure is felt on the capsule in the form of pain.
Note also that the supine position does not completely remove pressure from the disc, and it remains at 25 percent of the standing pressure. This is an important consideration because if a man weighs 150 lbs., there is still 55 lbs. of pressure acting upon the disc unit in the absence of traction. The significance of this will become apparent later when one considers other back pain programs’ exercises or the activity of chiropractors in which the supine position is utilized.
PATHOLOGICAL ANATOMY
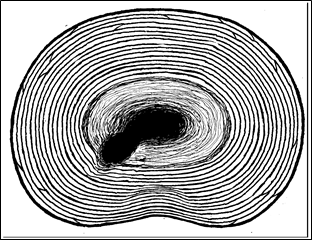
Figure 16; Cross-sectional schematic of disc looking down from above with herniated liquid Nucleus Pulposus.
These discs, being unique structures, break in a unique, pressure-induced, manner by herniating. When a disc is said to “herniate“, that technically means that a portion of the nucleus pulposus or other disc material has pushed through an anatomical structure meant to otherwise contain it. Many physicians refer to a herniation only when disc material is pushed through the outer capsule. This misuses the term because, then, they cannot rationally reconcile the painful events preceding a full protrusion or extrusion with their conception of a “herniation.” In fact, a herniation in the absence of a protrusion is very capable of causing pain.
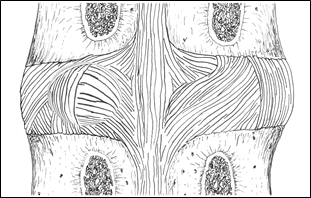
Figure 18; Posterior view of disc bulge to left.
In this book, a herniation is used in the universal, medical, definition as being anytime a portion of the anatomy protrudes through an abnormal body opening, even if that body opening is only a few innermost layers of the annulus fibrosus (See Figure 16).
When a disc is said to “bulge,” or “protrude” that should be taken to mean that the central material herniates or pushes through the annulus fibrosus to such an extent that it presses upon the ligamentous capsule causing it to deform and bulge outward (See Figures 17 & 18).
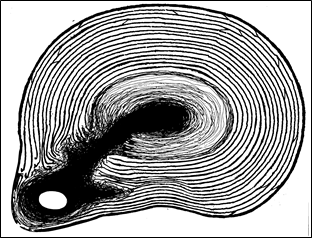
Figure 17; Cross-sectional view of disc bulge to left.
When a disc is said to “prolapse,” that is usually taken to mean that the disc material has herniated through the capsule (See Figures 19 & 20).

Figure 20; Disc prolapse to Left viewed from posterior.
When a disc completely herniates through the capsule it “extrudes,” the ordinarily central material tears through the ligamentous, peripheral, capsular structures and often enters the spaces adjacent to the spinal column (See Figure 21).
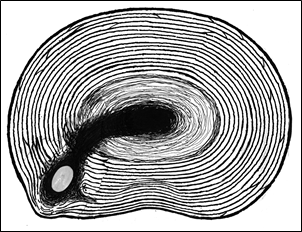
Figure 19; Disc prolapse to left with solidified nucleus pulposus herniating through capsule.
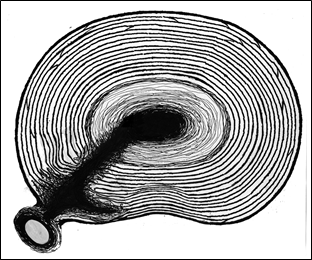
Figure 21; Disc extrusion with rupture of capsule.
Additionally, as a disc suffers multiple damaging events such as these, at many and varied sites within the discs, it can be said to “degenerate.” When this is the case, the bulk of the inner structural integrity is lost and the annulus fibrosus and nucleus pulposus can become a poorly functional conglomeration of broken fibers and pieces of cartilaginous debris. This “degenerative disc disease” usually comes later in life and is sometimes so severe as to have only the capsule functioning to connect one vertebral bone to the adjacent one. The concepts in this book apply to all these levels of damage but more so to that period of time when a total degeneration of the disc has not yet taken place. Even though this places limitations on the ability of The O’Connor Technique™ to benefit all disc related problems, nevertheless, the time in which relief can be expected is substantial and the principles still can be applied to relieve pain.
DISC HYDRAULICS/MECHANICS
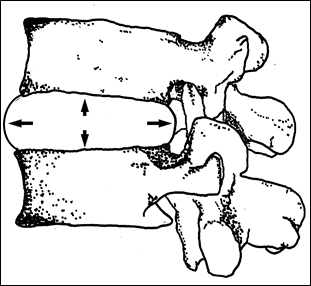
Figure 22; Balloon depiction of disc unit pressures in neutral position.
Since the majority of back pain emanates from problems related to the intervertebral disc, a discussion that is centered around the inter-relationships of anatomy, physiology, and mechanics is most pertinent. The effect of forces acting upon the spine which generate pain can be understood best by considering what physically occurs when forces are applied.
When a person is standing erect, the entire weight of the upper body above the pelvis is supported by the lumbar spine. Look at a skeleton, when the ribs end, the lumbar spine is the only structure left to support the weight. That means better than half the weight of the human body is resting upon the vertebral column in the upright position. This force is directed from above on every vertebral disc, compressing it. The bones are rigid, but the consistency of the discs more approach that of a liquid. The bones don’t physiologically compress, but the discs do.
The intervertebral disc’s management of compressive forces can be demonstrated by figuratively placing a liquid filled balloon between two vertebral bones (Figure 22). It is known in the laws of hydraulics that the pressures acting on a liquid are equal on any surface upon which the liquid acts. With both the anterior and posterior surface areas nearly the same, the pressure acting upon them is roughly equal when the material within the disc is largely a liquid.
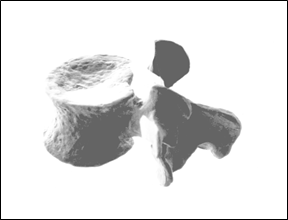
Figure 23; Bowl-shaped surface of disc area of vertebral body.
Now, consider what is happening when the body bends directly forward in flexion with weight on the vertebral column. The posterior aspects of the vertebral bodies separate and the space between them widens, increasing the surface area upon which the pressure acts, and causing the liquid center to bulge posteriorly. So, when the enormous pressures, as delineated above, are applied to the disc in anterior flexion they are felt by the posterior aspects of the annulus fibrosus and the capsule as in Figure 24.
When in flexion, the anterior component of the dish- or bowl-shaped (See Figure 23) disc containing surfaces of the vertebral bodies close while the posterior aspects of the bowl-shaped surfaces of the vertebral bodies open. In the anterior, the pressure is contained by two bony walls that have come together. In the posterior, the pressure is received by relatively weaker, stretched, ligamentous structures, causing the contents of the nucleus pulposus to protrude towards the back (posteriorly and peripherally as in Figure 24).
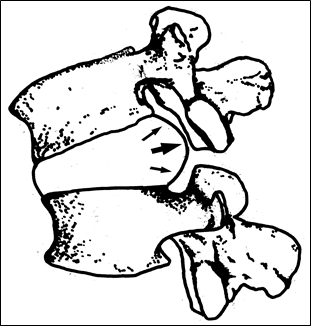
Figure 24; Balloon depiction of disc pressures in flexion.
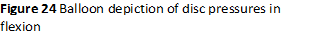 Like clapping jell-o with half-open cupped hands, the anterior aspects of the vertebral bodies are closed so the nucleus pulposus is forced posteriorly by the pressures exerted when these similarly bowl-shaped surfaces close. The “jello” has no alternative than to be squeezed out through the widest opening–the posterior.
Like clapping jell-o with half-open cupped hands, the anterior aspects of the vertebral bodies are closed so the nucleus pulposus is forced posteriorly by the pressures exerted when these similarly bowl-shaped surfaces close. The “jello” has no alternative than to be squeezed out through the widest opening–the posterior.
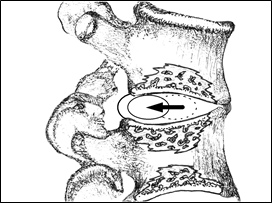
Figure 25; Movement of nucleus pulposus in weight-bearing flexion.
Under the tremendous forces generated during a flexion event ( as in lifting a heavy weight), the nucleus pulposus, its hardened center, and the more gelatinous components of the annulus fibrosus are all caused to forcefully move and expand posteriorly. The central disc material is caused to move away from the anterior compression force generated by the weight of the superior vertebral body pressing down on the bony surface of the inferior vertebral body. The vertebral bodies above and below the disc have concave surfaces which direct the central disc material posteriorly.
This central disc material (especially when it is not liquid as in an older person) often must move under the influence of these dish-shaped pressures and has nowhere else to go except posteriorly during weight-bearing flexion especially during traumatic or forceful events. It cannot move superiorly or anteriorly because it meets the bony surfaces of the vertebral bodies. The anterior component is closed by virtue of the flexion, and there is only one place for the hard central disc material and the liquid component to travel–peripherally and posteriorly, that is, away from the anterior compression induced by the weight-bearing flexion. The damage to the disc occurs when these forces are so great as to exceed the strength of the materials meant to contain them.
DISC HERNIATION PATHOLOGY
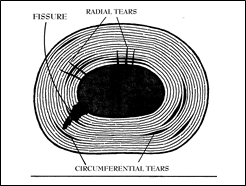
Figure 26; Radial and Circumferential tears in a youthful Annulus Fibrosus.
As these forces act upon the posterior elements of the fibro-cartilaginous laminations, the individual fibers are caused to deform and bow posteriorly outward. This, combined with the stretching occasioned by flexion’s separation of the posterior surfaces, rapidly takes these ligamentous structures to their full length. During rapid and excessive forces (such as in falls or heavy lifting) these fibers stretch beyond their tensile limit and tear. The first tears occur in the more central regions of the annulus fibrosus that have no nerve supply (so the damage is often not perceived) and that have no capillary blood supply (so that the cells of the inflammatory process cannot go inside to lay down scar or healing granulation tissue). These events constitute the initiation of the radial tear (Figure 26) and, thereupon, the degenerative process begins.
These tears can occur at an early age and, in and of themselves, go unnoticed due to the annulus’s lack of a nerve supply; however, the injury (if it occurs after the blood supply has retreated during the maturation process) never heals and the structural weakness most probably will remain for a lifetime. It seems strange, but a significant fall that lands a young person on his buttocks in flexion and causes no more than a mild discomfort, although easily passing as a few days with a sore back, can, in fact, set up the damaged disc unit for easier future damage of which the individual has no conscious awareness. Nevertheless, the tear is there, waiting for a future traumatic weight-bearing flexion event to result in advancing it to a frank herniation.
If the forces are sufficient, in injuries after an individual matures, the desiccated and hardened nucleus pulposus can itself fragment or cause the laminations of the inner annulus fibrosus to shatter and fragment. These materials once separated from their contiguous and attached cartilaginous structures become cut off from their nutrient supply and subsequently harden (when cut off from their water supply). Later, they can further break down and degenerate into what has been described as “crab meat” in advanced cases. They can also break off and become loose bodies within the spaces created by the fissuring and the tearing. This degeneration can become so severe that the disc loses its structural integrity causing one vertebral body to slide relative to the adjacent one. This results in a “listhesis” which can be painfully beyond the scope of this book’s ability to manage and necessitating a surgical fusion.
More commonly, these loose bodies, especially the hardened nucleus pulposus, upon the successive, forceful flexion events, can be forced further peripherally and extend the tearing. If the forces are directed linearly along the path of a prior injury and towards the periphery, this creates elongations in the existing radial tears (See Fig 27A,B,C) and extensions of circumferential tears (See Fig. 27 D), if the forces are created during a forcefully traumatic circumduction-like event such as twisting while lifting.
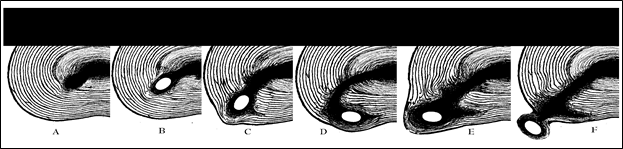
Figure 27; Sequential process of successive disc herniation leading to a sequestered fragment.
If the anterior compressive forces are generated more to the right side of the body, the opposite side of the posterior portion of the disc bears the brunt of most of the expanding force, that being the left side of the posterior aspect of the disc. This explains why a lifting injury caused by a heavy weight on the right side of the body causes the disc to be prolapsed or extruded more to the left. The above series of injuries (Figure 27) would have had to have been due to a flexion injury towards the right. It is not so much the twisting component of a lifting injury that results in damage, it is the fact that the more compressive force generated on one side of the body communicates more lateral force to the opposite posterior side where the ligaments are stretched to their maximum length already and cannot tolerate this force.
There is another reason why discs tend to herniate to one side or the other rather than directly posterior. As that force is felt more and more postero-laterally, the resistance of the ligamentous structures become weaker due to the gradual diminution of the posterior longitudinal ligament’s fibers as they anatomically become thinner at the lateral aspects of the discs. This is why a person should never attempt to lift a heavy weight off to the side of the body or twist while lifting (this action is well-documented to be the cause of frequent disabling back injuries). Also, twisting while lifting is damaging because the rotation of one vertebral body relative to another stretches the fibers more and predisposes them to breakage easier because a ligament that is already stretched to its limit is much more likely to rupture when force is applied than one which still has some play in it.
This phenomenon explains why it is a good recommendation that, when lifting, the weight should be placed as close to the midline of the body as possible and lifted directly upwards. In that way, the disc units are not in flexion, and the annulus fibers are not stretched by twisting or posteriorly directed pressure. Instead, the weight is sustained ideally by the shock absorber function of the disc while it is in line with the vertical axis of the spine. Therefore, if a weight has to be moved to a place to one side or the other, it is better to move the entire body by repositioning the legs rather than leaning to one side and twisting to accomplish the same task.
As described above, these forces have been measured by pressure transducers and they are quite phenomenal. They are tolerable in the young, flexible, well-hydrated discs of youth as evidenced by the nearly incomprehensible ability of a child to sustain falls in which they land on the buttocks with the spine flexed forward yet seemingly suffer no untoward consequences. The equivalent fall would most likely cripple an adult because, as a body ages, the liquid center of the nucleus pulposus becomes solidified as the cartilage component loses water with age and actually forms a solid disc-shaped structure. Also, up until the age of eight years, there are small blood vessels supplying the more centralized disc material which help heal it when it is injured. These are gradually obliterated as a person ages. By the time growth has stopped, the nucleus pulposus and the inner regions of the annulus fibrosus no longer have an active blood supply. Thereafter, only the outer most ligamentous structures have a blood supply and the rest of the disc must obtain sustenance from the diffusion of tissue fluid across the cartilaginous end plates. The central disc material becomes solidified and hardened with age probably due, in large part, to its loss of nutrient blood supply.
COMPRESSION FORCES
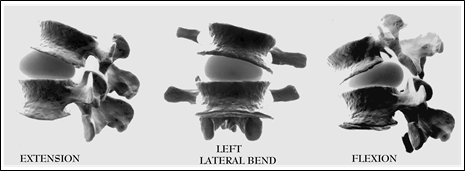
Figure 28; Balloon depiction of disc hydraulics.
It is important to fully understand the compressive forces acting upon the disc. Here, visualize, again, the two vertebral bodies separated by a balloon filled with water to reproduce the disc unit, illustrating the hydraulic and mechanical forces. As the top vertebral body is angled in any direction, such as in a flexed, extended, or lateral bending posture, it compresses one side of the balloon and the opposite side opens, causing the balloon to bulge to the open side. The balloon model accurately depicts the forces that act upon the discs because its liquid center, too, has nowhere else to expand except away from the compressive forces. As one flexes, extends, or laterally bends the spine, the forces are directed nearly identically to that displayed by the bulging of the balloons in Figure 28. An equivalent mechanical and hydraulic activity is occurring at each intervertebral disc whenever the spine bends away from an exactly vertical alignment. This is an important concept to understand because the direction towards which the nucleus pulposus bulges during traumatic events determines the direction and axis of the annulus fibrosus tears as well as the direction and axis that the nucleus pulposus contents would travel to herniate. For instance, if a fall or lifting accident were to occur when the spine was flexed more to the left, the herniating forces would be aimed towards the right posterior, and that would be the direction that the consequent radial tear would take as the contents of the nucleus pulposus herniate through the lamina of the annulus fibrosus.
Likewise, the magnitude of the force placed on the disc would determine the extent and depth of the nucleus pulposus’s movement; and, therefore, the degree of tear and/or consequent herniation. Lifting a small weight might not cause the nucleus pulposus to move much at all; however, a heavy weight can be seen to squeeze it with a lot of force and cause a lot of damage.
Archimedes said: “Give me a place to stand, and I will move the earth.” In the design of the spine, Nature’s reply has been: “Move the earth incorrectly, and I will make it so painful you cannot stand.” In order to understand the enormity of the forces that can be generated within the disc, one must look at the disc system’s relation to the spine in terms of the fulcrum and lever. The same principle that operates a nut-cracker or a claw hammer works against the disc when the forces are applied improperly during the act of lifting or falling in flexion.
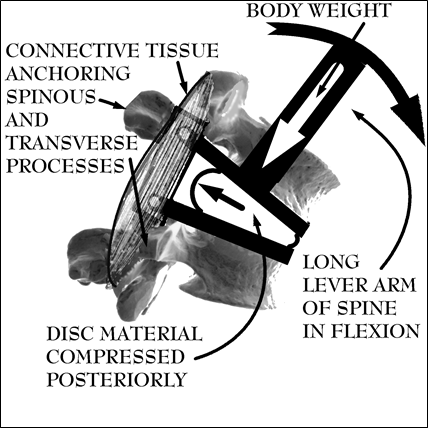
Figure 29; Fulcrum and body-weight generated compressive forces acting upon disc in weight-bearing flexion.
As seen in Figure 29, the disc system can be analyzed in terms of fulcrum and lever systems. When lifting in flexion, the muscles and ligaments of the posterior elements of the spine that perform extension and limit the range of anterior flexion serve as an anchor point because after they reach their maximum length, they can stretch no further. To insure that the ligaments of the posterior elements of the spine are not torn and that the body doesn’t fall forward during the lifting process, the muscles contract, serving to further anchor and act as a compressive force added to the weight of the body bearing down on the particular disc.
This connective tissue (muscle, tendon, and ligament combination) is depicted as a schematic muscle superimposed upon a rigid bar. The spine above the disc acts as the long lever arm of the fulcrum system. It can be imagined how with one end point of the “T-bar” (which is the entire vertebral bone above the disc) relatively fixed, the rest of the “T” rotates with the long lever arm that is the spine above the disc. During weight-bearing flexion the long lever arm rotates around a fixed point to create a posteriorly directed compressive force or squeezing pressure towards the posterior much like a fancy garlic press, nut-cracker, or claw hammer when the nail won’t budge. Incredible amounts of force are brought to bear on a small surface area. If one can see how a foot-long claw hammer can generate enough force to tear off the top of a nail, certainly a three foot spine can squeeze a rubbery piece of cartilage through a 2-3 mm sheet of sinew. If the reader jumps ahead to the Section on avoiding weight-bearing flexion, Figure 10 expands this diagram letting an obese clown show how these forces are magnified during lifting.
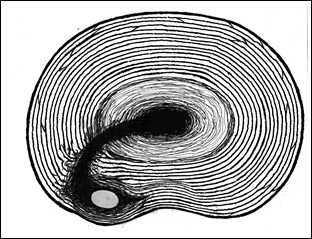
Figure 30; Disc material trapped in laminations of Annulus Fibrosus.
As mentioned before, with age and its consequent desiccation (drying out) also comes a decreased elasticity of the annulus fibrosus making it less liquid in character and more solid, predisposing it to breakage. As this solidification progresses with age, trauma has more likely a capacity to result in fragmentation. As this degeneration occurs subsequent to repetitive trauma, larger areas of central disc material become cut-off from contiguous tissue upon which it relied for its nourishment. These fragments then become less vital, more brittle, and literally degenerate, hence the term “degenerative disc disease.” As the solidified material of the nucleus pulposus is forced against the annulus fibrosus’s laminations as in heavy lifting in a flexed position, a fall with the back flexed, or even prolonged flexion with just the weight of the upper body, these fibers break, creating widened radial tears or fissures, allowing the hard, normally centralized, disc material (either fragments of solidified nucleus pulposus or the larger disc-shaped solidified nucleus pulposus itself) to migrate into spaces previously occupied by flexible, more liquid, deformable material.
Once these hard inner disc materials or fragments push their way through bands of the annulus fibrosus, they can stay positioned off center. So long as force is continually applied by the weight of the body, it can remain off center, often effectively becoming trapped between the broken concentric bands of the annulus fibrosus (Figure 30). These pieces of hard material can act as a fulcrum to create an effect that causes pain through mechanism described more fully later; but the more important consideration here is that it can cause pain even though it does not necessarily create an actual disc bulge that can be easily appreciated on imaging studies. These imaging studies often are interpreted as though the disc cannot be the problem because no obvious distortion of the capsule can be seen. In reality, the displaced disc material still is the problem. It is only hidden from easy diagnosis due to its failure to show a bulge or herniation on an imaging study.
This hardened nucleus pulposus can also tear sufficiently through the annulus fibrosus to create a pressure bulge in the posterior or lateral ligaments on the periphery of the disc. This is what is known as a disc bulge, protrusion, or prolapse. When the hard, normally centralized disc material is pushed completely through the ligaments, this is said to constitute an extrusion. See Figure 27 showing various and progressive degrees of damage.
For a moment I need to digress so that the reader understands what physical reality is being represented by these definitions. By defining the different herniation terms statically, there is an implicit assumption that these descriptions constitute an either/or phenomena. When no disc bulge or simply a mild disc bulge is seen on an imaging study, it is often incorrectly assumed that it is only a mild protrusion, incapable of being consistent with the patient’s described symptoms of pain, loss of function, or altered sensation. Such is not the case in nature where one is dealing with kinetic and flexible materials as well as reality wherein there is usually a spectrum of damage, at both the instant of injury as well as over time. Making an alternative assumption is a trap that sometimes taints the ability of individual medical doctors or research science in general to adequately portray or explain reality when applied to the individual. Often, the compulsive scientist is limited in his ultimate understanding by a need to rigidly and accurately define his terms so that there can be no confusion when attempts are made to reproduce the results. In the act of attempting to exactly define an entity that defies a static or rigid definition by virtue of its complexity and variability, errors in logic are the consequence. When applied in the context of practicing medicine, suffering usually results because these errors involve people.
For instance, if one were to do a study on the outcome of patients with protruded discs versus patients without protrusions, the protrusion definition and, hence, diagnosis must be fixed by some objective evidence. So, persons without evidence of protrusions on imaging studies are, by definition, eliminated from the study when, in reality, they may have suffered an extensive protrusion that has recoiled or spontaneously returned to a more centralized position by the time the diagnostic imaging is accomplished. It is important to understand that these pieces move, and, at the time of the study, the “protrusion” may not be protruded. It may only protrude when flexion combined with weight bearing forces are placed on the disc. The imaging studies might well have been done while the patient was in a reclining position with differing deformational pressures. So, for the purposes of the given study, this patient is not seen to have a protrusion and is likewise eliminated from the study’s consideration; or, worse, relegated to the realm of a malingerer if the doctor cannot reconcile the imaging study with the described degree of pain or disability.
The reason why I engage in this seemingly tangential discourse, here, is because there is a tendency to rely too heavily upon and simply equate what is seen (or, better, not seen) on an imaging study with the reality of the damage. If an imaging study has evidenced that a patient does not have a protrusion, that only means that at the precise instant the imaging study was accomplished, a protrusion was not seen. It does not mean that the patient has not suffered a protrusion event, and it may well be that the disc material only intermittently protrudes and spontaneously returns to the center with random motions.
An example of this phenomenon was inexplicably expressed in a medical journal wherein a physician reported that his back pain resolved when he flew his plane upside down. Essentially, he was unconsciously performing a traction maneuver that moved the displaced disc material centrally by a mechanism described at the end of this chapter. Also, numerous inversion traction devices have been marketed which inadvertently capitalize upon this mechanism; however, it is very uncomfortable to hang upside down. Nevertheless, the limited success of these methods, intentional or otherwise, demonstrate that the disc system is not static.
Disc herniations can produce a changing spectrum of symptoms depending upon the actual position of the herniated disc material, explaining why occupationally debilitated patients can, from time to time, be nearly symptom-free and perform activities in which, logically, their described disability would seem to be irreconcilable with their other performance. This explains why a person disabled from his employment as a brick-layer can be filmed by an insurance company’s private investigator playing basketball; yet still be legitimately disabled. Basketball can be played without much necessity for engaging in lumbar flexion, yet brick-laying requires it. Also, the disc material may be spontaneously centralized occasionally enough to engage in a non-flexing sport from time to time without significant pain. Yet, the instant that the patient goes back to his usual occupation, he flexes while carrying a weight, and the disc again decentralizes, returning him to pain.
Besides my own personal experience, to further support the reality of this phenomenon, I have seen at least two cases in which I have been able to closely examine the patients immediately after the injury (whereupon a clinical examination demonstrated that the nerve roots had been damaged at the instant of injury by compression against the vertebral bones due to a severe protrusion); yet the imaging studies (NMRI) portrayed only moderate disc bulges by the time they were actually done. Reconciling the clinical exams with the clinical outcomes forced me to conclude that they indeed have residual nerve damage; but, based upon the imaging studies, the protrusion did not involve the nerve at the time of the study. The erroneous conclusion was drawn that no nerve damage existed in the disability claim. The patient had definite nerve damage evidenced by atrophy of involved muscle groups; yet the back pain management “expert” physicians who evaluated this case relied nearly exclusively upon the imaging studies to determine that the patient was not truly disabled.
Not only does a kinetic spectrum of damage exist at the instant of injury; but it also exists over the lifetime of an individual. The manner in which successive damage occurs starts with any event that puts excessive forces on the disc. These forces, for the most part possessing a posteriorly directed vector, during flexion and weight-bearing, start by tearing small fissures in the innermost lining of the annulus fibrosus layers. This weakens that area and allows the nucleus pulposus to preferentially enter the space created. Successive traumatic pressure events then allow the radial tear to advance.
If the force is of sufficient magnitude, it can create large radial tears all at once; however, normally centralized elements of the nucleus pulposus, both liquid and solid, can also slowly continue to advance the radial tear over time and repeated small traumatic events. These tears can then dissect between laminations of the annulus fibrosus to create circumferential tears as laterally directed pressures likewise occur pushing the nucleus pulposus deeper into the separating layers of the annulus fibrosus. The mobilized elements of the nucleus pulposus can even be caused to move circumferentially between the laminations by a forceful, weight-bearing circumductional movement such as lifting while twisting (as mentioned above), even to the extent of becoming trapped by the bordering laminations of the annulus fibrosus (Figure 30). Once they are positioned to be able to do that, relatively small forces can dissect the laminations, widening the circumferential tears and allowing increasingly larger volumes of nucleus pulposus material to decentralize. This, then, predisposes the disc for a widening of the radial tears with the next weight-bearing, forced flexion event.
It is easy to visualize how this decentralized disc material can create tracts or tunnels by fissuring through layers of the annulus fibrosus, allowing the displaced disc material to move a number of ways either spontaneously or intentionally. It can continue to advance away from the center, follow the same path directly back to the center, or it can move circumferentially requiring a more complex series of movements to get it to re-centralize. This is when the problem is increased in complexity and much less likely to spontaneously resolve. In this instance, special consideration must be given to get it to re-centralize. The maneuvers of The O’Connor Technique™ are designed to re-centralize this aberrantly positioned disc material intentionally so as to reduce symptoms as soon as possible rather than to wait for random activity to generate equivalent forces in the ideal sequence over a protracted period. The method and means to accomplish this is discussed at length below.
This series of injuries can continue until the solidified nucleus pulposus actually leaves the confines of the capsule to become a sequestered or extruded disc fragment (See Figure 27F). Prior to this point, there is every reason to believe the mechanical problem can be managed and the damage prevented from advancing with The O’Connor Technique™: however, after the disc material escapes the capsule it usually can only be managed with surgical intervention if it produces loss of sensation, paralysis, or pain.
The intent of this chapter and the essence of The O’Connor Technique™ is to teach the back pain sufferer to understand the functional anatomy, forces acting upon, and the mechanics of the disc so as to be able to reproduce forces in an opposite direction to the original damaging forces and, thereby, re-establish the proper configuration of the disc relative to its containment structures. A person who masters this method can look forward to a future in which disc pain can be predicted, prevented, controlled, counteracted, and the spine protected from future injury and pain.
Recall the oxtail described above. It provides a nearly identical, natural, representation of the actual anatomy of a disc. I would seriously encourage the reader to go to a supermarket and find a package. It cannot be frozen, the meat must be fresh and the oxtail must be large because the smaller ones don’t adequately represent a disc approaching the size of a human disc. This is as close to a model of the human disc as is readily available since it represents the standard mammalian design. Of course, since the tail of the ox is not a weight-bearing structure there are small differences which must be overlooked. For this discussion, one is only interested in the anatomy and basic physical characteristics of the disc portion or the white, plastic-like, central portion.
Put your finger on the central white portion of the largest oxtail you can find. By continuously pressing down in the center with a finger and moving the hand in a circular motion one can often feel a central hardened area moving within gelatinous surroundings. This hardened center is equivalent to the central portion of the human disc system that hardens equivalently in the aged human condition. Now, if you imagine what would happen in the forced flexion position with downward pressure applied with the incredible gravitational forces that the back sustains, it’s easy to see how that hardened piece of cartilage-like material could break through and penetrate the circular, softer, concentric rings that are designed to keep it in place.
Look closely at the oxtail’s center and see those concentric rings of firm gelatinous tissue. If you really want to get the picture, make some oxtail stew out of them and cook them well-enough that the meat is falling off the bone. By biting into this material, you can appreciate how tough it is; and how it is indeed constructed of circular rings of cartilaginous tissue. By conceptually enlarging it in your mind, you can see how successive events of forced, load-bearing flexion can cause the radial tears that allow for the central material of the disc to move laterally and eventually escape the disc unit all together, resulting in an extrusion.
By picturing in your mind what would happen if that hardened disc material were to be traumatically forced against the rings of cartilaginous material by 500 lbs of pressure, you can envision how the layers would break and create a pathway (fissure) for the solid, central, disc material to traverse to the exterior leaving behind a canal of torn material. This is equivalent to a fissure (wide and long radial tear) in the human disc, and these are caused by a similar series of events wherein the central disc material (nucleus pulposus) is forced against layers of the annulus fibrosus breaking them to create a pathway through which the pieces of broken, hardened nucleus pulposus and fragmented disc material can freely travel.
Most people with injury-induced back pain, especially first-timers, have the type of tear with herniation, as opposed to an obvious disc protrusion or bulge. These herniations are usually invisible to the majority of medical imaging modalities. Discography (an X-Ray technique wherein dye is injected into the disc space highlighting the fissures created when the central disc material tears channels in the annulus fibrosus) is the most accurate means to detect these earliest of degenerative changes–tears or fissures of the annulus. These are difficult to detect by NMRI but, nevertheless, must exist in anyone with discogenic pain. Several studies support this finding. Due to the difficulty these tears have in being seen with imaging studies, multitudes of people are mis-diagnosed as having back sprain, muscle pulls, or pinched nerves. The presence of these fissures together with their herniated disc material can cause pain in any number of ways. This pain can be correlated and explained in terms of the mechanical anatomy.
CORRELATION OF MECHANICAL ANATOMY WITH DISC PAIN
Pain is an extremely interesting phenomenon, it can protect and teach while at the same time can intimidate and destroy nearly all enjoyment of life. Back pain is no different. Without adequate explanation or relevant education as to its source, mitigating factors, or potential duration, it can be interpreted as random, unpredictable, confusing, frightening, and apparently perpetual. When back pain strikes that can’t be alleviated in the usual time frame in which one is accustomed to seeing pain resolve, it can transform one’s life expectations into constant apprehension. Back pain is somewhat unique in the scope of body pains because it carries the added prospect of one’s potentially becoming disabled. Add to it the fear of losing one’s livelihood or the realistic potential for paraplegia and even a small injury can magnify any sensation to an inconceivably frightening level.
Psychologists tell us that the stress induced by pain can be markedly better endured and tolerated so long as it is not perceived as random, it is made controllable, and predictable in both its onset and termination. Any pain can be tolerated much more easily if the seeming randomness is explained and understood. The purpose of this section is to lift the “blindfold” on the most common form of spinal pain by defining its source as discogenic (originating in the disc), familiarizing the sufferer with its various manifestations, and, through education, make the unseen source of pain understandable, manageable, predictable, and ultimately preventable.
To remind the reader, it is well-established that the nucleus pulposus and the inner portion of the annulus fibrosus have no nerve supply. Only the most outer portion of the disc unit, the ligamentous capsule and peripheral aspect of the Annulus Fibrosus, has sensory innervation. Some misuse this anatomical fact to assume that there should not be pain associated with either the tearing of a solidified nucleus pulposus through the laminar rings of the annulus fibrosus or the degenerative process in general. To a certain extent this is true and explains why people often relate that during the twisting or lifting event that they know initiated their pain, they just felt a pulling or a “pop.” Only later did they gradually experience the sharp, debilitating pain. Also, people within hours of a whip lash injury describe the same experience. Immediately (minutes) after the trauma, they are a little sore, but the real grinding and immobilizing pain often comes hours later or the following morning when they wake up and try to move their neck. This is perhaps the most paradoxical aspect of spinal trauma. One would think that, if significant damage was occasioned, it would be immediately apparent and obvious at the scene of the trauma as in the case of a motor vehicle collision. After all, whenever someone pulls a muscle, breaks a bone, or sprains a ligament, the pain is apparent immediately.
One must consider, when trying to make sense out of the pain, that the entire disc system has very little tolerance for misplaced parts. Simply because one cannot feel the actual damage being done as the hardened components of the nucleus pulposus herniate through the annulus fibrosus doesn’t mean that once they come to rest, placing direct pressure on the outer ligamentous bands of the annulus fibrosus or posterior longitudinal ligament, that they won’t induce pain as the pain receptors within those ligaments are excited and the inflammation process begins.
DIRECT PRESSURE PAIN
First, tears of the annulus allow the de-centralized disc material to move towards the disc’s periphery and put direct pressure on the ligamentous capsule that surrounds it. Movements putting the affected part of the spine in forward flexion can be seen to actually squeeze the hardened nucleus pulposus or other pieces of disc material posteriorly to put direct mechanical pressure on the posterior aspects of the capsule (See Figure 31). These capsular ligaments are very well-supplied with nerves and are quite capable of generating severe pain.
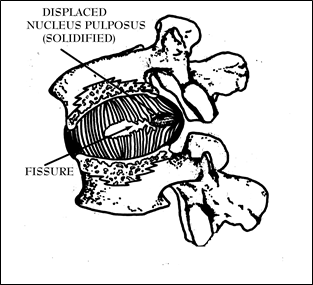
Figure 31; Cut-away view of disc unit in flexion showing a displaced nucleus pulposus.
Also, the residual liquid component of the nucleus pulposus can participate in this pain scenario, especially when weight-bearing flexion causes the liquid component of the disc to exert hydraulic pressure on the posterior peripheral capsule. Considering what is occurring anatomically when trauma tears free the solidified nucleus pulposus and forces it through layers of the annulus fibrosus, there are areas of liquid nucleus pulposus that now have the capability of entering the fissure and hydraulically adding to the pressures that are felt on the posterior capsule. The hardened nucleus pulposus as well as its liquid counterpart are free to dissect through the fissure to reach the sensitive capsule to generate pain when the nerve-supplied ligaments are stretched.
When flexing in the weight-bearing condition (weight-bearing flexion) hydraulic pressure or mechanical pressure on the nucleus pulposus forces it (or fragments of desiccated cartilaginous material) into the outer bands of the annulus fibrosus and posterior longitudinal ligaments, and pain is the consequence (See Fig 31). This effect can occur instantaneously or over a prolonged period of time due to successive events of pressure. This type of pain can be looked upon as originating from direct pressure applied to the capsule’s ligaments.
The pressure on and damage to the peripheral ligamentous component of the disc (the capsule) and the posterior longitudinal ligament are probably the most important contributors to pain in the disc system and are largely responsible for the majority of pain attributable to back pain in general. Others may argue pulled muscle, sprain, arthritis, or some other mechanism, but, since the time I have been able to manually reduce disc herniations or put “in” de-centralized disc material with The O’Connor Technique™, my experience has shown me that the greatest component of spinal pain originates in the direct pressure placed on the exquisitely innervated joint capsule that surrounds the disc unit when decentralized disc material exerts pressure on those ligamentous structures. I “know” this because, once I have relieved this pressure through manipulation, the pain relief is usually instantaneous. In fact, it is very uncommon for me to have a back pain patient that I cannot prove has disc disease as the source of pain by virtue of my ability to relieve it. This leaves me with no other conclusion to draw.
As elaborated above, the peripheral ligamentous structures surrounding the disc, the joint “capsule,” contains the sensory nerve fibers that tell where the upper body is in relation to the lower body. This innervation is the reason why you can stand upright and a baby (who is too young to have these pathways functional) falls over, even if only seated. It takes a high density of sensory fibers to be able to discriminate extremely subtle movements. When this same density of sensory receptors is applied to pain sensors, it implies that a little stimulation can go a long way in producing pain. That small amount of stimulation can come from a relatively small piece of displaced disc material pushing against the capsule or when, off-center, it creates a fulcrum effect in concert with the adjacent surfaces of the vertebral bodies.
These parts of the body rarely feel pressure or experience trauma during the youthful formative years of neurologic development due to their deep location in the body and their being surrounded by protective muscles that prevent their routinely experiencing painful stimuli. Therefore, when forces induce pain, it is registered by the brain as a novel phenomenon which usually translates to pain the severity of which has never been experienced by the average person any prior time in their life.
For this reason, annular tears can be very painful; yet patients with just these tears (in the absence of a bulge or protrusion) are often dismissed as having psychogenic pain motivated by secondary gain, mostly because discography is not done to demonstrate the true pathology. However, doctors don’t routinely order discography and for good reason. It is a dangerous and invasive procedure. Only highly trained and qualified physicians are willing to stick a needle into the disc because it is painful and risky. If the radiologist is only a couple of millimeters off, a nerve root could be injured leading to paralysis. Since it is so difficult to identify these tears with non-invasive methods like X-Rays, CAT, or NMRI scans, the most convenient but alternative, erroneous, diagnoses are usually made instead.
FULCRUM EFFECT PAIN
The other major contributor to mechanical discogenic pain can be appreciated by considering what happens when, over time, with successive small injuries, a major lifting injury, or a traumatic flexion event the central disc material breaks its way through the layers of the annulus fibrosus but doesn’t necessarily reach the peripheral capsule. The broken fibers of the annulus can close like one-way doors behind it, trapping the normally centralized disc material in an off-center position. The hard disc material then acts as a fulcrum. The vertebral body and the portion of the disc above it acts as a lever with the weight of the body providing the moment arm’s force during flexion.
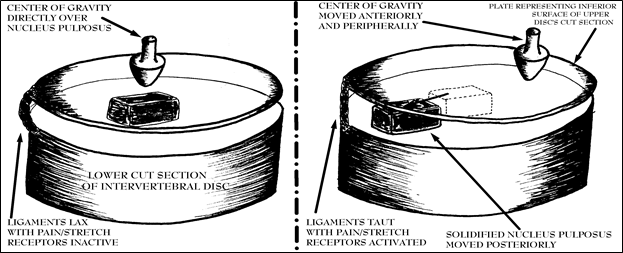
Figure 32; Fulcrum effect of disc when center of gravity is changed and solidified nucleus pulposus is displaced.
This phenomenon is not difficult to comprehend. Figure 32 schematically portrays a disc cut in horizontal cross-sections. The inferior surface of the superior section of the disc is shown as a transparent plate resting above the inferior component of the intervertebral disc. The displaced disc material or hardened nucleus pulposus is represented by a “brick” that rests between these virtual surfaces. The figure on the left describes the neutral (normal) situation where the center of gravity (fat arrow) is directly above the nucleus pulposus. In this configuration, the ligaments are relaxed and no pain is felt so long as the body is balanced directly above the center of the disc.
The figure on the right shows the condition in which some previous traumatic forward flexion event has displaced the hardened nucleus pulposus towards the posterior periphery. Then, the act of moving the center of gravity towards the periphery (as shown in the drawing on the right by the movement of the fat arrow), in this case equivalent to antero-lateral flexion, puts an inferiorly directed force on the “plate” causing it to teeter on the “brick” (the solidified nucleus pulposus) which stretches the “rope” (representing a ligament with pain/stretch receptors). When the force of the weight of the body acts with a fulcrum effect upon the component of the disc (the “plate”) immediately above the hardened nucleus pulposus the forces stretching the ligaments become quite substantial. I term this fulcrum effect pain.
In the presence of a herniation, during my examination for diagnostic purposes, when I cause patients to change their center of gravity anteriorly (in a forward flexion directly away from the site of pain while standing, they easily agree that the pain is stretching due to the mechanical or hydraulic pressure on the posterior capsule. This pain is the pain of direct pressure. However, they then agree the pain is wedge-like when I keep them bent and circumduct them until the point that the fulcrum effect stretches the capsular ligaments adjacent to the displaced disc material. They recognize the pain as if something was physically wedged in their back when I then shift the center of gravity around to the other side of the herniation by circumducting them in the opposite direction. The slightest increases, beyond the point where pain begins, increases that tension and seems to magnify the pain exponentially. This configuration creates an effect similar to what happens when a pencil is placed in a door hinge wherein any attempt to close the door results in damaging forces.
Even though the pencil is
relatively small, shutting the door can warp the metal hinge due to the power of a fulcrum/lever system. The same fulcrum/lever effect is occurring in the damaged disc unit.
Circumduction moving from antero-lateral flexion to lateral extension (leaning successively through a circular, clockwise, range of motion) of the spine at the problem disc level causes pain by a fulcrum/lever mediated stretching of the peripheral capsular ligaments. As in the diagram analogy, moving the center of gravity along a circumferential path clockwise along the rim of the plate, successively puts and keeps tension on the ligaments such that, the closer one moves the center of gravity towards the brick, it becomes necessary to relax the degree of extension to get over the “hump” created by the wedged, hardened, nucleus pulposus. Similarly, moving the center of gravity around in a counterclockwise direction would have an equivalent effect upon other ligaments equivalently situated to the displaced disc material on the opposite side. The effect of this type of action is discussed in depth in the section on diagnostic circumduction wherein the pain and arrest in circumduction can be used to determine the position of the displaced disc material. Feel free to return to this drawing to understand that concept as well.
Just as the tiny pencil placed in a door hinge can stop the door from closing, so, too, can a small piece of cartilage-like material, when off-center, cause pain as the surrounding ligaments are stretched by a fulcrum effect. Attempts to force movement in spite of the misplaced disc are often met with excruciatingly sharp pain. The pain is often immobilizing because no matter what direction you turn or what position you assume other than balanced directly above the nucleus pulposus, the pain increases.
These factors explain why, during an acutely painful back event, the sufferer can neither bend forward to any extent, move towards the painful side, nor extend enough to stand up straight without increasing the pain to an intolerable level. In any of these movements, the hard, off-center disc material can serve as the fulcrum for any of a number of possible levers and moment arms created by the cartilaginous and bony surfaces contiguous with that disc and the displaced disc material. Depending upon which of the other sites on the adjacent surfaces of the vertebral bodies is farthest from the displaced disc material, it becomes the moment arm. The site with the shortest distance becomes the lever. The lever then can stretch peripheral ligamentous tissues with forces much stronger than would otherwise be generated without the lever/fulcrum effect.
For instance, let’s assume that the solidified disc material is displaced off-center to the midline posterior in the neck not enough to cause a direct bulge or protrusion, however, enough to impede competent movement. When the patient tilts his head forward and to the right, the displaced disc material, now turned elevated fulcrum, causes the left posterior peripheral ligamentous elements to be stretched with far greater force than they ordinarily would be caused to be in the disease-free condition. This causes a stretching pain to be felt to the left of the displaced disc material. The same thing happens when the head is tilted to the left, only this time the stretching type pain is to the right of the herniated piece of disc material.
As above in, Figure 32, the forces acting on the disc’s ligaments can be equated with a rope (about the length of the brick’s height) tied to the edge of a circular shaped board and secured to a platform. If a brick were placed in the center of the board and someone were to stand on the end of the board farthest from the rope, the rope would probably not break because the end of the board where the weight was applied would hit the ground before that could happen. However, moving the brick closer and closer to the rope’s site of attachment, the board (just as the displaced disc material moves closer to the peripheral ligaments as it is displaced posteriorly and peripherally) increases the fulcrum effect so that, when it is nearly touching the rope, even small amounts of force on the far end of the board can be seen to be capable of snapping the rope.
I have ascertained to my own satisfaction that this mechanism of pain is the predominate cause of a condition known as torticollis or “wry-neck syndrome.” Usually it is seen more often in children; but is also seen frequently in adults; but their necks don’t seem to go into as much of the uncontrolled spasm as is routinely seen in children. Rather, the adult is most of the time unable to look over the shoulder to the same side as the displaced disc material. However, it is not unusual for the condition to be chronic or even perpetual. The disc material is usually displaced more laterally than posteriorly, and it causes the sufferer to turn his face away (due to contraction of the sternocleidomastoid muscle) but bend his neck towards the side of the herniation (due to a combination of same-sided paracervical muscle spasm and an attempt by the individual to keep the weight of the head’s center of gravity directly over the displaced central disc material. To anterior flex the neck to the opposite side as the displaced disc material creates pain so the head and neck are kept rigidly immobilized partly because of spasm and partly because nearly any movement off of the center of gravity causes extreme pain.
It appears to some that muscle spasms are the source of the problem. So much so that, recently, some doctors have reportedly improved the condition by injecting a muscle relaxant into the sternocleidomastoid muscle; however, I fear this practice is too dangerous and ineffective because, technically, it only treats a symptom of the problem and not the origin. Alternatively, I have found it is the fulcrum effect of de-centralized disc material stretching the peripheral ligaments that initiates the spasm. The disc material displaced is most likely liquid nucleus pulposus in the child and/or solidified nucleus pulposus in the adult which has herniated off-center. This herniation, I have found, after careful history taking, to be usually due to a flexion injury, either in the immediate past or the remote past (that only has acutely re-herniated due to so much as sleeping in the wrong position).
On occasions too numerous to count, acting upon these assumptions by using The O’Connor Technique™ I have been able to non-traumatically and immediately reduce the subluxation with manipulation rendering the patient free of pain and restore full range of motion. This success is contrasted to reports in the literature of this condition lasting for years in the absence of definitive management. In fact, there are so many people in this country that have this untreated condition that they have formed a society.
Understand that the above described intervertebral disc fissure-facilitated mechanism of disc material displacement pain can occur over a long period of time with repeated nearly identical flexion injuries or instantaneously with a sufficiently powerful force. After repeated events that progressively damage the annulus fibrosus, even a seemingly small force can result in debilitating pain since the disc can be poised at any time to suddenly travel the same damaged route to reach the intervertebral ligaments. This explains why people can be doing something as apparently innocuous as taking out the trash early in the morning and “put out” their backs, resulting in a permanently painful back condition requiring surgery. Such is the case in many incidents which are usually not believed by the patient’s doctor to be sufficiently traumatic to result in a disc protrusion or herniation.
You see, in cases like this, where someone comes into the doctor reporting that a sneeze or simply waking up and putting on shoes initiated a severe back pain event, the doctor reasonably assumes that no major damage could have occurred to ligamentous or bony structures because the forces applied were inconsistent with the ability to damage these characteristically tough structures. However, the original event that predisposed to the presently painful one, may have been a fall as a teenager or an auto accident years prior that resulted in only moderate, transient pain. The disc material in the first injury never moved enough to become trapped; but it damaged the annulus enough to create a pathway for future advancing of the injury. Few people realize that the cartilaginous material that comprises the annulus doesn’t heal or repair itself over time. Once it is fractured, it doesn’t even scar. It remains perpetually broken and capable of allowing the central, hard disc material to repeatedly migrate along a previously created pathway. This helps explain why studies show that 40% to 85% of patients will have recurrences of back pain within a year after their initial episode., and nearly one third of patients with low back pain have a relapse within 3 years of the initial episode. Each event in which a radial tear is created makes it more likely for a fissure to be created and another, future, painful event to occur. As time goes on, cumulative injuries predispose to progressively severe disease.
This phenomenon also explains why “degenerative” lumbar disc disease is said “to progress as a series of pathophysiological events, beginning with asymptomatic fissuring and fragmentation within the disk.” It is not widely appreciated, difficult to accept as fact, and worth repeating here that a significant radial tear can occur in the annulus fibrosus without inducing a reasonably commensurate amount of pain because these structures do not have nerves supplying them. The age-solidified nucleus pulposus, gradually and eventually, through repetitive trauma, herniates through successive layers of the annulus fibrosus, followed by prolapse of this fibrocartilaginous material into the spinal canal or the neural foramen. The pain comes only when the surrounding ligamentous component of the disc sustains pressure, stretching, or inflammation whenever the irritation is sustained.
It is the fulcrum effect which is often to blame for the pain pattern experienced in motor vehicle accidents which is commonly understood as “whiplash.” A peculiar phenomenon which I have observed is the reported pain pattern seen during accidents in which a rear-end collision is sustained by the patient. They frequently state that the pain wasn’t present at the scene of the accident. Most of the time they only report a stiffness and discomfort which later becomes debilitating hours later or the next day when they wake from sleep.
Often assumed to be an effort to pursue personal injury claims, after the incident when the prospect of monetary gain has been considered and can be realized, I have found (to the contrary) that the pain is real; and it is the fulcrum effect inducing the pain at a time distant from the actual injury because only later is tension to be repeatedly placed upon the intervertebral ligaments as the injured disc unit undergoes weight-bearing flexions, extensions, and circumductions in the conduction of normal, natural, activities of daily movement.
You see, the actual damage induced in the collision is often a tearing of the annulus fibrosus as the nucleus pulposus is displaced. Recall that the annulus fibrosus has no nerves, so when a fissure is created at the instant of trauma, it is only perceived as a crunching sensation followed by a subtle stiffness (often unrecognized) or a lost range of motion (especially in extension) at the scene of the accident. Within minutes of the accident, these sensations are easily overlooked due to the psychological trauma, adrenaline influence, and no physical evidence of trauma at the neck or neurological deficit. After all, the neck is usually not struck by any object during the collision. However, the displacement of the disc material towards the periphery (herniating usually posteriorly and laterally) is not necessarily sufficient to actually result in an immediate disc bulge. It is only late, as the ligaments begin to have the fulcrum effect exerted upon them and they undergo microscopic tears leading to inflammation, do they become painful.
I have come to understand this because I have repeatedly been able to immediately relieve this type of pain in patients (with no intention of capitalizing upon the accident) through manipulation, restore their range of motion (by replacing their disc material), and prevent them from becoming members of the “Wry-Neck Society.”
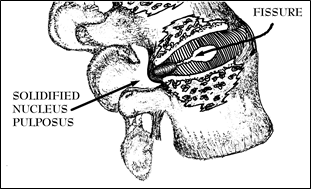
Figure 33; Herniated Nucleus Pulposus positioned to exert both a direct pressure and fulcrum effect.
There is also a combination type of pain that is experienced when the centralized disc material (the solidified nucleus pulposus, the broken fragments of the annulus, and/or the liquid component of the nucleus pulposus) bulges or protrudes to the rims of the adjacent vertebral bodies due to a herniation that causes the capsule to significantly deform and bulge posteriorly. In this case, the pain comes from the disc material causing both a fulcrum effect and direct pressure pain by its being trapped during the act of extension (See Figure 33). The decentralized disc material is positioned so far peripherally that it is actually pinched or squeezed by the vertebral body’s rims. This, too, puts pressure on the capsule and results in pain.
CRIMPING PAIN
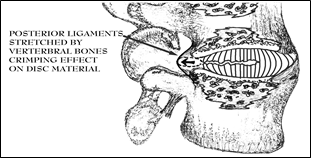
Figure 34; Cut-away view of disc showing crimping effect of vertebral body’s rims coming together during extension on prolapsed piece of disc material.
When extending in the weight-bearing condition (weight-bearing extension) extension is often only allowed until the fulcrum effect is experienced because pain stops the movement; however, another condition that is closely related to the pain of the fulcrum effect yet is more appropriately considered as a constant direct pressure pain is when the displaced disc material has protruded to the point where extension of that disc unit causes a crimping of the prolapsed disc material. The crimping or pincer-like action happens when the disc material is pushed beyond the rim of the vertebral bodies and enough of it is outside of the circumference of the plateau portion at the rim of the vertebral bones to not allow it to move anteriorly in the presence of the body weight’s compression forces (See Figure 34). Often, a fragment of displaced disc material is lodged in this prolapsed position; and the act of weight-bearing extension traps and pinches it further posteriorly. This type of pain usually requires a protrusion or bulge-type herniation to be present, but one isn’t absolutely necessary if the greater part of an ideally-sized piece of disc material is situated immediately peripheral to the point where the lips of the vertebral bones oppose each other such that their approximation when extension is occasioned creates a bulge.
RADICULAR PAIN
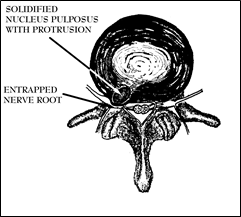
Figure 35; Protruding disc material causing direct entrapment and compression of a spinal nerve root.
Radicular pain comes as a result of an extruding, protruding or prolapsed disc fragment coming into direct contact with a spinal nerve root (See Figure 35). Since the sensory component of the nerve roots travel down to the areas to which they supply innervation, pressure on these large roots can cause pain to appear to be coming from the places where the nerve travels. This type of pain is a searing, burning, or electric shock-like sensation that is often associated with a definite extremity weakness and loss of muscle strength because the spinal nerve contains fibers that carry, sensory, pain and motor (muscle movement) signals. Since this type of pain if persisting, signals a nerve root compression syndrome and most likely will result in immediate surgery to remove the piece of disc material that is compressing the nerve, it will not be focused upon too heavily here except to elaborate that there are definite nerve root impingement syndromes described to explain the consequent loss of sensation, pain and motor loss depending upon the particular nerve root that is damaged. If the reader experiences this type of pain, this book is not a wise solution until one has been rejected as a surgical candidate by a neurosurgeon.
REFERRED PAIN
None of these mechanisms thus far explains why the hip or leg hurts when the lower spine is supposed to be the problem or why the shoulder hurts when the cervical vertebrae’s discs are supposedly the source of the pain when there is clearly not a protrusion seen on an imaging study. The more commonly experienced Referred Pain reveals that the central nervous system isn’t as smart as you think. In some ways, it is very unsophisticated, especially with novel events in which it has not been given time or capacity to become accommodated. By way of example, when a thorn is stuck in the leg while walking, initially, the brain recognizes that the leg hurts. You cannot determine anything more specific than the right lower leg has pain. The next thing you do is attempt to localize the pain by feeling the area and reproducing the pain by touching the affected site to convince yourself that indeed, that specific point is where the pain originates.
Next time you have a small injury, think about the pain. Finger pain can seem like the whole hand hurts until focus is directed at the actual source to pin-point the site. Most times it is necessary to feel around at length to determine the exact site of a particular pain’s origin. In order to localize and identify pain, it is usually necessary to bring in other modalities of the central nervous system such as sight, movement response, and touch in order to localize it. Well, when the actual source of the pain is hidden deep inside a part of the body that cannot be felt, seen, touched, or knowingly moved in such a manner to identify the true source of pain, the brain is forced to make, often incorrect, assumptions.
Take for instance a painful condition that most people have heard about. Heart pain is so rare to the central nervous system’s experience that, when it occurs, it is often thought of and felt to be in the arm. This is explained because the nerves to the arm are embryologically developed from the same pathway as the heart’s nerves. So, the mind, trying to determine the pain’s origin, concludes that the pain must be coming from the arm because the nerves are being excited from the same general pathway as the arm. Since heart pain is so rare, the mind assumes that the pain must be coming from somewhere else more accustomed to receiving pain signals. After all, most heart pain suffers are older than forty years old. The central nervous system has been living that long without pain from that area and has good reason to not “believe” pain could be originating there. So, it is not unreasonable for the brain to make an alternative “assumption”.
When it comes to spinal pain, the brain is equally confused. This was documented by a study in which subjects were injected with irritating solutions into the facet joints at various levels. They were unable to determine which level was being injected or whether the disk or facet joint was being injected.
I am convinced that a similar pain pathway confusion frequently occurs when the nerves of the intervertebral disc’s capsule are stimulated. Depending upon what level of inter-vertebral capsular ligaments are involved, take for instance L5-S1, the pain message emanating from this disc space is similarly accepted by the brain to have origination from the areas of the more customarily stimulated nerves’ embryological distribution. The large spinal nerve root that exits the spinal column (that eventually supplies innervation to the muscles, skin, and joint of the hip) sends a small branch to the disc area, the Recurrent Sino-Vertebral Nerve (See Figure 10.) Both pain and proprioceptive impulses travel to the spinal cord and on to the brain through this nerve. When painful stimuli excite the small nerve from the disc’s capsule, the impulse travels along with other fibers coming from other sites supplied by that particular, larger, spinal nerve. These pathways are so closely related that the mind frequently accepts the pain as having originated from the other sites which have been more accustomed to managing pain sensations throughout the life of the individual. Depending upon what spinal nerve is pertinent, the sensations, upon reaching the brain, are often accepted as having come from those areas of the body also innervated by that spinal nerve root in which the impulses from the disc also travel.
When the disc capsule’s pain receptors are excited and pain impulses are produced, one can’t very easily put one’s finger on the actual site of pain at the L5-S1 disc level to convince the mind it is in error as in the thorn example given above; so, the central nervous system makes the incorrect “assumption” that the hip is what hurts and that site is from where the pain is mistakenly registered by the brain as having its origin. These areas correlated with the distribution patterns of spinal nerves are well-known and mapped out as sclerotomal, dermatomal, myotomal patterns corresponding to their respective spinal nerve levels. These patterns are delineated in more exhaustive textbooks for professionals and need not be reproduced here; but, ideally, by identifying what area the dull aching pain comes from at rest, one should be able to tell which disc is the source of pain. In reality, there is so much overlap of areas, the opportunity for further confusion is so rife, and that degree of exactitude is neither necessary nor realistically achievable by the lay persons that I have elected to dispense with its discussion.
The O’Connor Technique ™ makes such a pursuit academic. An individual can learn to correlate their own particular pain patterns with specific disc units simply by moving the spine and paying educated attention to where and when the pain is felt. Then, when that pain recurs, it can be assumed to be from the particular disc with the herniation. This will become more pertinent and apparent when, later, the reader is taught how to diagnose their own disc herniation because he/she will be able to specifically move their spine to find the actual discogenic source of pain regardless of where the pain radiates or refers.
Also, of note, something interesting about referred pain is that if you stimulate the area that appears to hurt, such as with a massage or rubbing, the pain temporarily disappears as if the mind, then, is saying: “Oh, the pain can’t be coming from there because now I’m touching it and it is not being reproduced; therefore it has to be coming from someplace else.” Then, the instant that the massage or stimulation stops, the pain recurs because the brain again returns to making an incorrect assumption like that elaborated above.
To better understand this type of pain, one should know that referred pain usually has limitations. It seldom travels beyond the elbow or knee. Rarely, in my experience, has referred pain gone below the knee in a lumbar disc problem or beyond the elbow in a cervical disc herniation when a nerve root is not involved. When it does, that can be a sign that the pain is radicular and caused by the actual pressure of a prolapsed disc on the nerve that passes through that segment of the spine. Radicular type of pain is usually described as “burning” whereas the referred pain is more often described as a “dull ache.” Whenever pain seems to involve a strip that runs the entire length of the leg or arm, or is accompanied by actual weakness, that is a bad sign, made worse if it is accompanied by weakness of that same muscle area, and there should be no delay in seeking out a physician to determine if further studies or an operation is necessary to prevent destruction of the nerve.
A common source of not overtly obvious shoulder or leg pain is from an intervertebral disc referring the pain. Without other cues, the mind often cannot differentiate pain originating from the stimulation of a nerve at any point along the distribution of that nerve. The brain may register as the source of pain any site of stimulation whether it originates at the level of the nerve as it exits the spinal column, nerves that travel in the same bundle, or from the area innervated normally by the nerve.
As an experiment to demonstrate this phenomenon, the next time something hurts on your legs such as a bite, scratch, or any narrow area of trauma, without looking or touching, close your eyes and try to figure out exactly where the pain is coming from by just closing your eyes and focusing on the site. Your first impulse is to touch the area to determine the exact locality of the pain. You will probably realize, until this is done, you feel pain simply coming from a broad general area on the leg. In order to convince your mind where the exact location of the pain is, it is usually necessary to feel the area, actually reproduce the stimulation by pressing on the area of pain, and convince yourself that you have located the exact point of its origin.
Now, consider what happens when a disc or a nucleus pulposus puts pressure on the ligamentous bands on the periphery of the annulus fibrosus. There is no way that you can touch the disc with your hand to convince your mind that you have located the exact origin of the painful stimuli. Consequently, the mind must resort to guess work. The brain must assume the pain is coming from the nerves that innervate that area of the body to which the nerve being stimulated supplies nerve function.
In the case of the Lumbar region, the nerves are the same ones that go to the hips, buttocks, and legs. The pain is dull and no matter how much you touch the area that aches, you can’t make it hurt more or reproduce the pain by touching areas from which the pain appears to come. If the pain were truly coming from the hip joint, moving just that joint should increase the pain, but it doesn’t, neither does pressing on what seems to be the pain site. In fact, quite often, rubbing or massaging those areas stop the pain momentarily because the stimulation convinces the brain that that area cannot be the source. However, as soon as you stop, the pain returns.
As a pertinent aside, this paradoxical phenomenon can be explained by the Melzack and Wall gating theory of pain because sensory impulses travel faster than pain impulses and, when they beat the pain impulse to the spinal cord, they preferentially stimulate the nerves that travel to the brain by a gating mechanism. The brain receives the sensory input before it accepts the pain impulse.
Evolutionarily, this makes some sense since when running away from a predator, the organism is better served by a nervous system that physiologically ignores pain while allowing sensory input to have preference. It is apparently more a selection advantage to know where your feet are running than whether they hurt or not. Another model for this reality comes from the frequent experience of men in combat who describe no pain sensations while distracted by complex sensory input enabling them to continue functioning despite massive wounds.
The sensations of touch, temperature, stretching (so-called proprioceptive impulses), and vibration travel in very fast fibers. Consequently, these impulses arrive at the spinal cord’s “gate” earlier and get through faster and more often than the pain impulses that travel in slow fibers. This explains why hot packs and ice packs both relieve pain. Unfortunately, they do very little to modify or heal the true source of the pain since neither heat nor cold can reach the disc.
This information comes as scant consolation since one must first understand what is causing the pain to alleviate it. Towards this purpose, let us assume that a patient has hip pain on the right side. Many of my disc patients actually do not complain of low back pain per se, but describe it as predominately hip pain which accompanies the lumbar pain. This is also the case of the shoulder’s relationship to the cervical spine.
They rarely have pain in the actual hip joint upon testing the range of motion of that joint so long as the back is prevented from moving during the testing. When traction is applied to remove pressure from the protruding disc, the first thing they notice is that the hip pain is relieved; and the spine becomes the site of pain. Only after having they do a Diagnostic Circumduction Maneuver (to be explained later) in which they convincingly reproduce the pain and their movement is arrested, can I determine the position of the disc protrusion. Once the site of pain is identified, I put the disc back “in” with a centralizing maneuver. When they achieve relief of their hip pain, I can be certain that the disc was the source because that is the only area that was mechanically altered. Because I usually prove this is what is occurring by successfully putting the disc back “in” and the patient walks out without hip pain, I am forced to conclude that the pain relief would not have occurred unless the spine was the origin because that is the only area that had been mechanically altered.
I have also had a continuous opportunity to study this phenomenon on my own disc pain for years. This first-hand knowledge gives me a great deal of insight into my patient’s experiences and the intricacies of spinal pain in general. When my disc is “out” the pain is more in the superior buttock than the spine. Upon completing a maneuver, the hip pain is likewise extinguished.
So, in evaluating your own low back pain, with The O’Connor Technique™ you can learn to recognize hip or buttock pain as originating from the disc material pressuring the nerve that refers pain to the hip. You can determine that the true source of the pain is coming from the spine by moving the spine in a very specific manner which will be discussed later in the description of the Diagnostic Circumduction or “The O’Connor Test.” When doing the diagnostic and therapeutic maneuvers described later in this book, be cognizant of what particular movement accentuates the pain and what particular therapeutic maneuver decreases it. Usually, the diagnostic circumduction, when attempting to go to a full posterior extension, will be accompanied by arrested motion when the actual area of the displaced disc material interferes with the movement of that particular disc unit. Just as the point is reached where you feel as though, if you continued without letting up on the extension the pain would be unbearable, your extremity should start feeling the pain, and the sensation of something obstructing the movement should occur. This is the point where the surfaces of the vertebral bones interfacing with the discs are beginning to put pressure on the displaced disc material. It usually stops you from circumducting further and gives the sensation that if you could just move the right way the pain would be relieved. It is often described as a “catch” in the back, like something is caught and prevented from moving further. That is the most characteristic component of disc pain that differentiates it from other types of pain. The following chapters go into much greater depth so don’t stall here concerned that you have missed the point.
MUSCLE PAIN
Certainly, other sources of pain in the back do exist. People occasionally “pull” or “strain” the muscles in their back; but this is associated with a different type of pain. The pain of a “pulled” muscle (actually torn) in the erector spinae group is usually not associated with extremity pain or if it is, it is a pain that is reproducible and increased when the affected muscle is manipulated. Recall, the referred pain from the disc usually is made to feel better while being manipulated. The pain of a torn muscle is identified by tenderness (pain upon touching) of that specific muscle when it is palpated. When manual pressure is put on the torn muscle it becomes immediately more painful. So, with a backache, it is simple enough to test for actual muscle tenderness at the time of the injury, if it is present this gives reasonable evidence to conclude that the source of pain does not come from a disc. However, in my professional experience, a pulled muscle in the back is a rather uncommon event. However, pain in the muscles is not necessarily that uncommon because muscle pain can come from secondary spasm due to a herniated disc.
The pain of muscle spasm is sometimes hard to differentiate from pain due to a muscle tear because both are accompanied by a generalized hardening and swelling of the affected muscles. Spasm often follows a back injury in which a disc is herniated because that is the body’s protective mechanism. The spasm can be expressed as an intermittent jerking with jolts of pain or continuous, depending upon whether or not the pain comes in short, rapid bursts (such as when a damaged ligament is stretched for an instant with movement) or sustained for long periods (such as when disc material is persistently deforming a ligament). By spasming, the segmented animal splints that area of the body so that injured midline structures are protected. Recall what happens when you pinch a worm, it curls towards the pinch. If you ever get the opportunity to handle an new born baby, place it face down with its stomach in the palm your hand so that its bare back faces you and its hips can move but each leg is straddling your arm. By running your finger down the back about one inch lateral to the spine you will see the Landau reflex. The baby will contract the erector spinae muscles automatically on the same side that the stimulus is applied. There is very little difference between this reaction and the reaction that occurs when a painful stimulus is applied to the spine later in life. The erector spinae muscles automatically and involuntarily contract towards the side of injury. When this contraction is sustained because the pain is continuous, the muscles go into a prolonged contraction or what is commonly referred to as spasm.
The best way of differentiating the pain of spasm from the pain of a pulled muscle is to feel the muscle itself. Usually, the torn muscle will be tender at the site of the tear immediately after the injury. The muscle that is painful due to prolonged spasm may become tender along its entire length but it does so only at a time distant to the injury and along the entire length of the involved muscle. The pain of both are increased when flexion away from the side of the pain is accomplished.
In order to differentiate between muscle pain versus disc pain, the job is much easier. When in extending to the side of the pain in the presence of muscular pain, the pain is reduced. Think about it, muscle pain from tearing is decreased when tension is taken off of the muscle and increased when tension is put on the muscle. So, when in a passive (without the activation of the muscles) extension position towards the herniation’s side, a pinching of the disc should increase the pain. When passively extending to the side of pain, the erector spinae muscles will be relaxed to that side and result in less pain when the pain is due to a muscle tear. Additionally, there is usually no actual arrested motion in the presence of muscle spasm or tear. With a herniation, the displaced disc material physically stops the act of circumduction. A torn or spasmed muscle might be painful to move, but it will not stop the spine from circumducting.
INFLAMMATORY PAIN
A discussion about the sources of pain in the disc system would not be complete unless Inflammatory Pain were included. Whenever an anatomical structure in the body sustains trauma, especially constant or repetitive friction due to abnormal pressures placed upon a component, inflammation usually occurs. This inflammation results from chemicals produced by the white blood cells that migrate to an area to facilitate the repair of damaged tissue. When displaced disc material is mechanically impinging upon structures that have a blood supply, cellular damage is occasioned. As the disc material abuts against the ligamentous structures, inflammation is created. Unfortunately, as long as the ligaments are being irritated by the continuous pressure of the displaced disc material, the inflammation will persist. It stands to reason that the pain of inflammation will also not resolve until the mechanical problem of the decentralized and aberrantly placed disc material is solved. Later in the book, methods designed to remove the disc material from pressing against the ligaments will be elaborated. Once the friction is relieved, the inflammatory component can be managed successfully.
LIGAMENT TENSION PAIN
When a disc has sustained repeated trauma to the extent that the annulus fibrosus has become extensively cracked and fissured, the nutrient supply of fluids and oxygen to the cartilaginous material becomes compromised and the disc undergoes what is called degenerative changes. Over time, these changes cause the nutritionally unsupported tissues to dessicate (dry out), degenerate, and collapse. This is recognized on imaging studies as disc space narrowing with a loss of “height” observed in the disc space. The vertebral bones can then dislocate by sliding relative to one another, coming close enough together to rub or catch at the peripheral edges.
After a disc has severely degenerated for many years, the majority tissue that once constituted the actual disc can become simply a ground up mass of non- or poorly functioning material that has lost the bulk of its structural integrity, leaving the ligamentous capsule as the disc’s only anatomical structure joining the two vertebral bones. In this advanced disease, the displacing vertebral bones can cause the ligamentous capsule, the intervertebral ligaments to be stretched when one lip of bone comes to rest more inside the concave region of the vertebral bone surface. This causes pain not dissimilar to the direct pressure pain because in either instance, the pain emanates from tension on, the stretching of, and the microscopic tearing of the intervertebral ligaments. This effect is capable of causing severe pain. On the contrary, having experienced the sensation of the vertebral bones contacting each other and knowledgeable of the lack of enervation to bone (since the nerves are only located in the outer covering or periosteum), it does not appear that extreme pain is generated from bone rubbing against bone, although the sensation is not particularly pleasant .
Even though this level of disease occurs, for the most part, in ageing bad backs; the mechanical actions of maneuvers and principles still can effectively be used to relieve pain because the movements designed to replace displaced disc material also re-position and re-align the vertebral bones along their vertical axis. At this stage, though, sustained relief may only come with surgical fusion; however, by persistent application of the The O’Connor Technique™ the degenerated disc unit can be expected to remodel in a markedly less painful configuration.
ADDITIONAL SOURCES OF PAIN
Finally, without question, back pain originates from and accompanies many other disease states. Spinal stenosis (narrowing of the spinal canal), ankylosing spondylitis, arthritis, spondylolisthesis, cancer, fracture, trauma, infections, etc.; however, in my personal medical and orthopedic experience, the overwhelming majority of spinal pain originates in the disc and is due to some consequence of disc herniation. Those orthopedists, chiropractors, and medical doctors are entitled to their opinion when they attribute acute (rapid onset) or recurrent back pain to pulled muscles, ligament sprain, lumbar strain, sciatica, sacro-ileitis, spasm, etc. because those events do occur but not nearly with the frequency of disc herniation. However, they, more often than not, cannot make a convincing, logical argument with some form of objective proof to demonstrate the accuracy of their diagnosis because they seldom are required to design one. They are rarely held to the standard that their diagnoses be correct nor are they exposed too much of an untoward consequence if their diagnosis is erroneous. They simply make their best guess based upon what they assume to be fact, then rely upon Nature to remedy that which they cannot even adequately describe. This may sound like an indictment or a criticism; however, it is not. It is simply a statement emanating from a realistic assessment of the widespread, contemporary, lack of understanding about discogenic pain.
TRACTION FORCES
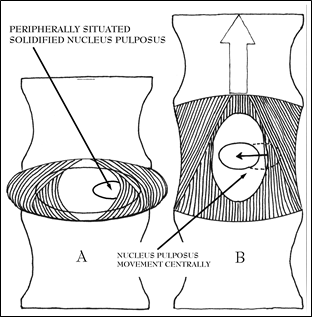
Figure 36; Tightening of peripheral ligaments and creation of negative pressure moving nucleus pulposus due to traction.
Another means of differentiating whether the source of pain originates in a disc or from some other source is that a slight amount of traction can transiently relieve disc pain. In muscle tears, “sprains,” or inflammatory arthritis of a joint, the isolated act of traction, in and of itself, will induce pain. Traction in the presence of a disc herniation will noticeably reduce the most severe component of the pain–the hydraulic or mechanical pressure induced component caused by the herniating or prolapsing material pushing against the ligamentous peripheral annulus, the capsule, or the posterior longitudinal ligament.
In keeping with the balloon analogy used before to describe compressive forces, one needs to understand an equally important decompressive force that can act upon a disc. That force is mediated through traction. One can imagine what would happen to a liquid filled balloon that has been glued to the vertebral bodies similar to the manner in which the disc is anatomically secured in the natural condition. When the vertebral bones are separated along the vertical axis (or in other words, pulled apart along their longitudinal axis, superiorly and inferiorly), as would occur when a person hangs or is put in traction, the contents and periphery of the balloon would move centrally due to the negative pressure generated and the tension placed on the balloon’s walls. Likewise, in the natural mechanics of the disc, when traction is applied the disc contents are both drawn by central negative pressure from the relative vacuum created as well as pushed centrally by tension-generated inward directed pressure as the peripheral ligamentous structures are stretched and tightened.
A dilemma arises, however, in that, before one can solve the mechanical problem of disc pain, a means must be found to convincingly and precisely identify and define the pain as originating from a mechanical problem then devise a means to insure that the mechanical component of the pain is truly no longer acting. The following Chapter on Diagnosing Disc Disease deals with how that is accomplished.
1. Perey O: Fracture of vertebral end plates in the lumbar spine. An
experimental biomechanical investigation. Acta Orthop Scand (Suppl) 25:10, 1957.
2. Nachemson AL: In vivo discometry in lumbar discs with irregular nucleograms. Acta Orthop Scand 36;426,1965.)
3. Borenstein DG, Wiesel SW, LOW BACK PAIN Medical Diagnosis and Comprehensive Management, 1989, W.B. Saunders Co, Philadelphia, London, etc.
4. Walsh TR, Weinstein JN, Spratt KF, et al. Lumbar discography in normal subjects: A controlled, prospective study. J Bone Joint Surg. 1990;72A:1081-1088.
5. Op.Cit., Endnote #3;p.14.
6. Sasso RC, Cotler HB, Guyer RD, Evaluating low back pain: The role of diagnostic imaging, The Journal of Musculoskeletal Medicine, May 1991:21-37.
7. Valkenburg HA, Haanen HCM. The epidemiology of low back pain, in White AAIII, Gordon SL (eds) American Academy of Orthopaedic Surgeons Symposium on Idiopathic Low Back Pain, St. Louis, CV Mosby Co, 1982:9-22.
8. Troup JD, Martin JW, Lloyd DC, Back pain in industry: A Prospective Survey, Spine (1981) 6:61-69.
9. Deyo RA, Back Pain Revisited: Newer Thinking on Diagnosis and Therapy, Consultant, February 1993: 88-100.
10. Vlok GJ, Hendrix MR. The lumbar disc: evaluating the cause of pain. Orthopedics, 1991; 14:419-25.
11. Deyo RA, Loeser JD, Bigos SJ. Herniated lumbar intervertebral disk. Ann Intern Med, 1990;112:598-603.
12. Mooney V, Robertson J. The facet syndrome. Clin Orthop 1976;115:149.